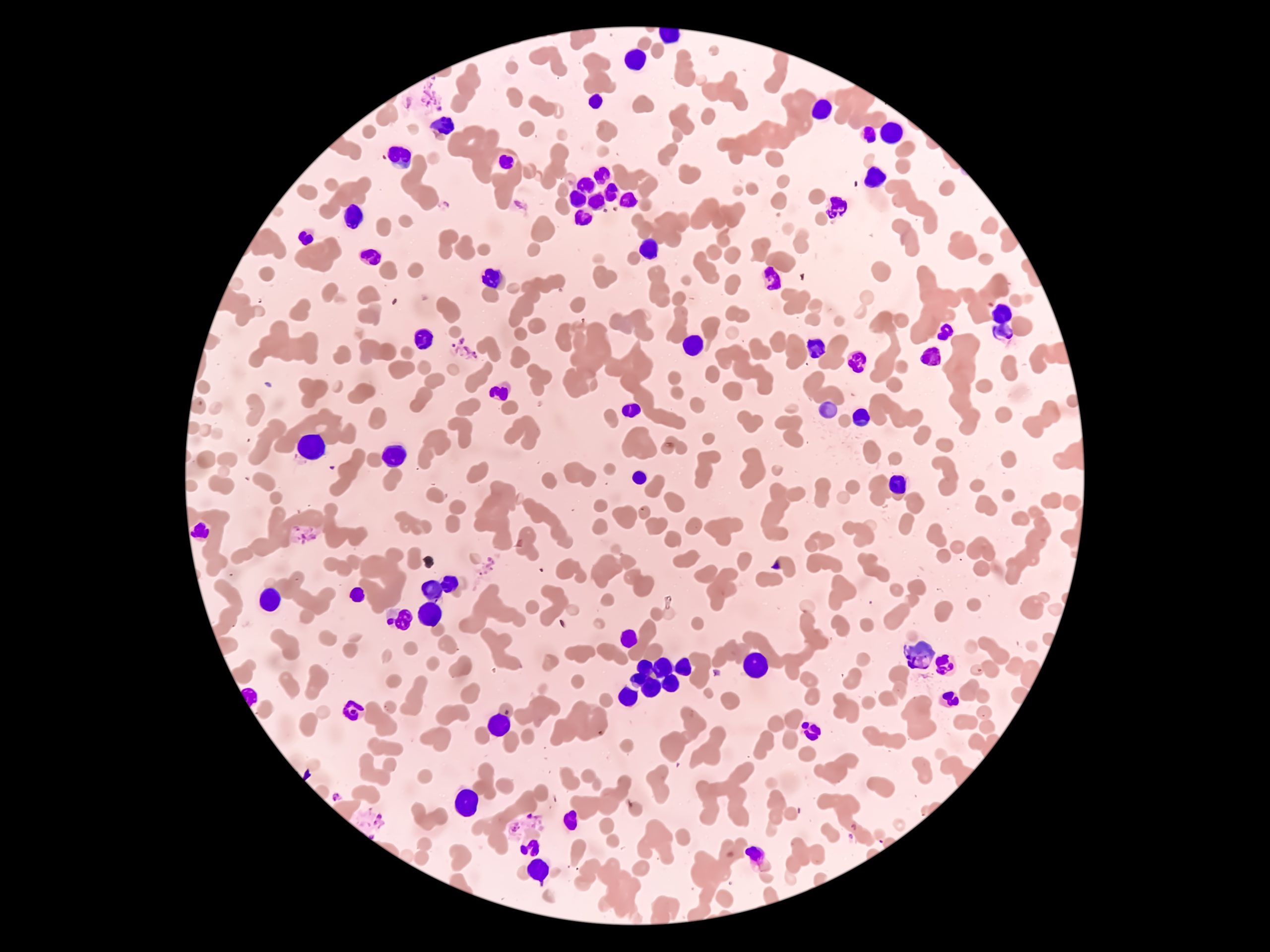
Waldenström macroglobulinemia (WM) is a rare blood cell cancer characterized by the presence of lymphoplasmacytic lymphoma (LPL) cells in the bone marrow and production of a monoclonal immunoglobulin M (IgM) paraprotein. WM can typically be monitored without treatment in asymptomatic patients, although approximately 50% of patients may develop progression requiring treatment within five years.
The most common mutations associated with WM are MYD88, CXCR4, ARID1A, and CD79B. Recurrent somatic mutations in MYD88L265P and CXCR4 have been reported in 90% to 95% and 30% to 40% of patients with WM, respectively. Wild-type MYD88 (MYD88WT) tumors are associated with worse prognosis, while acquired CXCR4 mutations (CXCR4MUT) are not.
Because WM is considered incurable, an important treatment consideration is optimization of quality of life, which is most effectively pursued by achieving a balance between disease control and minimization of treatment toxicity and side effects.
Standard Management Approaches: Rituximab-Based Combinations
According to the National Comprehensive Cancer Network Clinical Practice Guidelines, the preferred frontline regimens are rituximab-based combinations, including bendamustine and rituximab; bortezomib, dexamethasone, and rituximab; and dexamethasone, rituximab, and cyclophosphamide.
The initial treatment should be customized to the individual situation based on factors such as the patient’s fitness, baseline comorbidities, desire for fixed treatment duration, disease bulk, presence of cytopenias, level of IgM, and the presence or absence of CXCR4 and MYD88 mutations.
BTK Inhibitors
Ibrutinib, the first U.S. Food and Drug Administration (FDA)-approved drug for treatment of WM, is an orally administered, covalent Bruton’s tyrosine kinase (BTK) inhibitor shown to trigger apoptosis in WM cells with MYD88L265P. Zanubrutinib is a newer, more selective covalent BTK inhibitor than ibrutinib.
Both FDA-approved BTK inhibitors are highly active in WM. However, only zanubrutinib appears to induce responses in MYD88WT and CXCR4MUT disease; therefore, zanubrutinib may be preferred over ibrutinib in MYD88WT disease and when a short time to major response in CXCR4MUT disease is desired.
Acalabrutinib, tirabrutinib, and orelabrutinib are second-generation, highly selective, covalent BTK inhibitors that are not yet FDA approved in this disease space.
Although well tolerated, BTK inhibitors are associated with known off-target side effects, including cytopenias, specifically neutropenia. Thrombocytopenia was more frequently reported with ibrutinib than the second-generation BTK agents. The randomized ASPEN trial reported a lower rate of cardiac events (ie, atrial fibrillation and hypertension), diarrhea, and bleeding with zanubrutinib versus ibrutinib. It also demonstrated that the incidence of infection is equivalent between agents despite a higher rate of neutropenia with zanubrutinib.
BCL2 Inhibition with Venetoclax
Venetoclax, a B-cell lymphoma/leukemia-2 (BCL2) inhibitor, was first investigated in a phase I study, which enrolled 106 patients, only four of whom had WM; however, all four patients with WM attained a partial response with a median duration of response of 25 months. In WM cells, in vitro and ex vivo, apoptosis was induced after treatment with venetoclax, and venetoclax sensitized WM cells to ibrutinib, indicating that upregulation of BCL2 may be an important mechanism of resistance to BTK inhibition.
Combinations
To date, just a handful of studies have demonstrated superiority of multiagent regimens over single-agent treatment. A phase II trial reported at the 2021 American Society of Hematology Annual Meeting & Exposition investigating the addition of bortezomib to bendamustine and rituximab in patients at first relapse (after a rituximab-based regimen) was able to meet its primary efficacy endpoint of an absolute increase in 18-month progression-free survival from 50% to 65%. These results demonstrate that combining multiple active agents into a single regimen can lead to superiority compared to standard-of-care with a tolerable safety profile.
The combination of ibrutinib and venetoclax has also been shown to have synergistic activity and be well tolerated in chronic lymphocytic leukemia and mantle cell lymphoma. Trials are now underway investigating the combination of venetoclax and ibrutinib in WM to be administered during a two-year limited time frame (fixed duration therapy).
Future Directions: Mavorixafor
Mavorixafor is an investigational, small-molecule, selective antagonist of the CXCR4 receptor being developed as an oral treatment for patients with congenital warts, hypogammaglobulinemia, infections, and myelokathexis (WHIM) syndrome, a rare, autosomal-dominant primary immunodeficiency.
In the first human study to treat WHIM syndrome, mavorixafor demonstrated a favorable toxicity profile, as well as proof of concept that it effectively restores white blood cell mobilization from the bone marrow. The drug also sensitized CXCR4MUT WM cells to ibrutinib, leading to a multicenter phase Ib trial investigating the safety and activity of the combination of mavorixafor and ibrutinib, which is now underway. To date, of the 10 patients with confirmed MYD88L265P and CXCR4MUT disease evaluable for efficacy analysis, 100% responded to this treatment, with three partial responses and one very good partial response.
Other Novel Targets and Pathways
Newly identified cell-signaling pathways and novel targets for WM are currently being investigated to further expand the treatment landscape for the disease. These include proteasome inhibitors, immunomodulators, phosphoinositide 3-kinase inhibitors, BCL2 antagonists, CXCR4-targeting agents, anti-CD20 monoclonal antibodies, and anti-CD38 monoclonal antibodies.
Despite the rapidly evolving field of immunotherapy in oncology, few studies have investigated immune-stimulatory agents or cellular therapies in WM. A phase II trial is currently underway investigating pembrolizumab, a humanized monoclonal anti-programmed cell death-1 antibody, combined with rituximab in patients with relapsed/refractory WM.
Similarly, while chimeric antigen receptor (CAR) T-cell therapy has revolutionized the treatment landscape for hematologic diseases, there are no data in WM. Despite cost and safety concerns, the possibility of long-term remissions after only one dose of CAR T-cell therapy for WM may offer a prospective treatment for medically fit and younger patients.
Finally, given the strong expression of surface antigens such as CD20 and CD19, bispecific antibodies and antibody-drug conjugates may be of interest in this disease state and warrant further exploration.
For the time being, novel agents targeting BTK and BCL2 have shown to be safe and effective in patients with WM. Future studies will focus on developing fixed-duration combination regimens with these novel agents aimed at increasing durable responses while minimizing toxicity and cost.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.