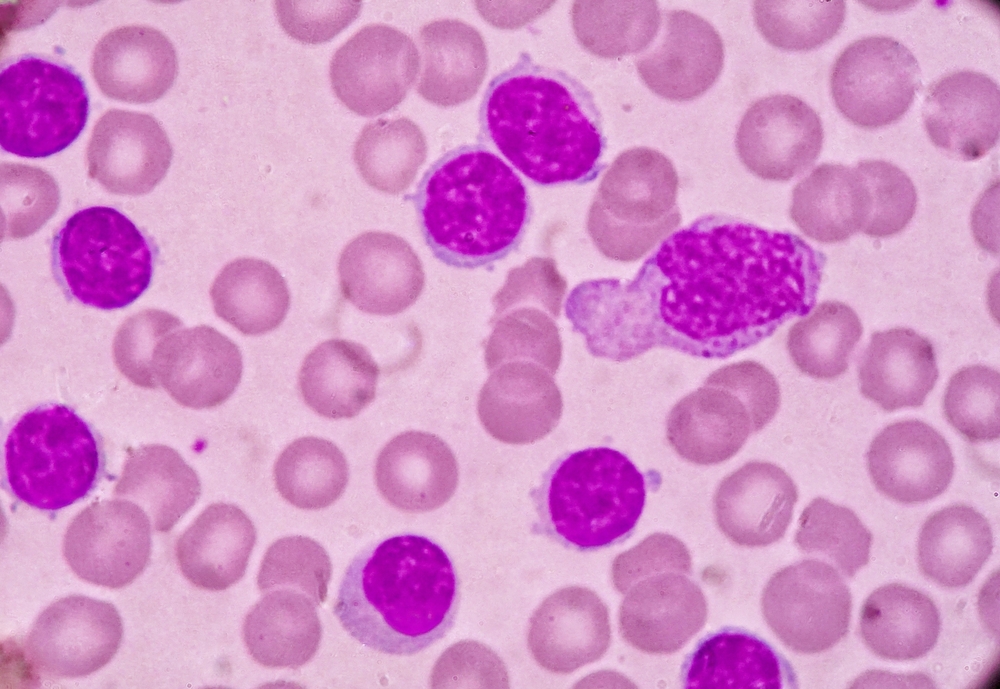
After nearly 4 years of follow-up, acalabrutinib monotherapy maintained efficacy compared with standard-of-care regimens in patients with relapsed/refractory chronic lymphocytic leukemia (CLL), according to updated findings from the ASCEND study presented at the 2022 ASCO Annual Meeting.
Results from the primary analysis of the study (median follow-up, 16.1 months) showed that acalabrutinib had superior efficacy compared with idelalisib plus rituximab or bendamustine plus rituximab regimens.
The multicenter, randomized, open-label, phase III study enrolled 310 patients with relapsed/refractory CLL who were randomized to receive acalabrutinib 100 mg orally twice daily (n=115) or investigator’s choice of idelalisib 150 mg orally twice daily plus rituximab 375 mg/m2 for one cycle then 500 mg/m2 intravenously (IV) for eight total infusions (n=119) or bendamustine 70 mg/m2 plus rituximab 375 mg/m2 for one cycle then 500 mg/m2 IV for six total infusions (n=36).
Median patient age was 67 years (range, 32-90 years), 15.5% had del(17p) mutation, and 73.5% had unmutated immunoglobulin heavy-chain variable (IGHV).
After a median follow-up of 46.5 months in the acalabrutinib group and 45.3 months in the investigator’s choice group, acalabrutinib significantly prolonged progression-free survival (PFS; primary endpoint) compared with investigator’s choice (median, not reached vs 16.8 months; P<.0001). PFS at 42 months was 62% with acalabrutinib versus 19% for investigator’s choice.
In patients with del(17p) mutation, median PFS was not reached with acalabrutinib versus 13.8 months with investigator’s choice (P<.0001). In patients with unmutated IGHV, median PFS was not reached and 16.2 months, respectively (P<.0001).
Median overall survival (OS) was not reached in either cohort; 42-month OS rates were 78% with acalabrutinib versus 65% with investigator’s choice. Overall response rate was similar between the cohorts: 83% and 84%, respectively.
Adverse events led to treatment discontinuation in 23% of acalabrutinib-treated patients, 67% of idelalisib plus rituximab-treated patients, and 17% of bendamustine plus rituximab-treated patients. In both the acalabrutinib and investigator’s choice arms, adverse events of interest included all-grade atrial fibrillation/flutter (8% vs 3%), all-grade hypertension (8% vs 5%), all-grade major hemorrhage (3% vs 3%), and grade ≥3 infections (29% vs 29%).
“These results confirm that long-term acalabrutinib treatment as a chemotherapy-free regimen maintains efficacy and continues to be safe for patients with CLL who either relapsed after or stopped responding to previous treatments,” the authors concluded.
The study was sponsored by AstraZeneca.
Reference
Jurczak W, Pluta A, Wach M, et al. Acalabrutinib versus rituximab plus idelalisib or bendamustine in relapsed/refractory chronic lymphocytic leukemia: ASCEND results at 4 years of follow-up. Abstract #7538. Presented at the 2022 American Society of Clinical Oncology Annual Meeting, June 3-7, 2022.




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.