
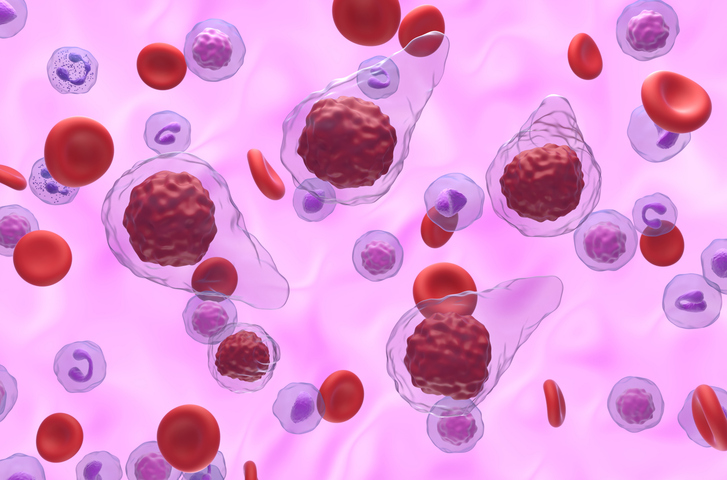
A 3D model was used to analyze the effects of interferon alfa (IFNa) in the bone marrow (BM) microenvironment, which could be helpful in understanding fibrotic progression in JAK2V617F mutation–positive myeloproliferative neoplasms (MPNs) and treating accordingly, researchers reported at the 65th ASH Annual Meeting and Exposition in San Diego, California.
For the study, researchers analyzed high-purity and clonal patient-specific induced pluripotent stem cell (iPSC)-derived endothelial cells (ECs) with JAK2V617F mutations, compared with wild-type JAK2 controls, and evaluated vasculogenesis. The proliferation rate was significantly higher for JAKV617F-mutated iECs compared with wild-type JAK2 iECs, according to Madeline Caduc, MD, of the Department of Hematology, Oncology, and Stem Cell Transplantation at the University of Aachen in Germany, and colleagues.
Treatment with fedratinib (a JAK2 inhibitor), anagrelide (a platelet-lowering agent), or venetoclax (a BCL2 inhibitor) significantly reduced iEC viability, but ruxolitinib (a JAK1/2 inhibitor) and interferon alfa did not have this vascular toxicity. Further analysis showed that interferon alfa did not alter vascular tree formation, but it significantly impaired neoplastic vasculogenesis, Dr. Caduc and colleagues noted.
“Our model is a valuable tool to decipher the poorly investigated impact of IFNa on the BM microenvironment,” the researchers concluded. “In addition, its translational and scalable properties (eg, by integrating primary or iPSC-derived hematopoietic cells) will allow us to study the impact of additional drugs on MPN-associated fibrotic transformation of the BM.”
Reference
Caduc MJ, Grasshoff M, Ernst S, et al. Interferon-alpha impairs neoplastic vasculogenesis in a 3D iPSC-based model of JAK2V617F+ myeloproliferative neoplasms. Abstract #742. Presented at the 65th ASH Annual Meeting and Exposition; December 9-12, 2023; San Diego, California.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.