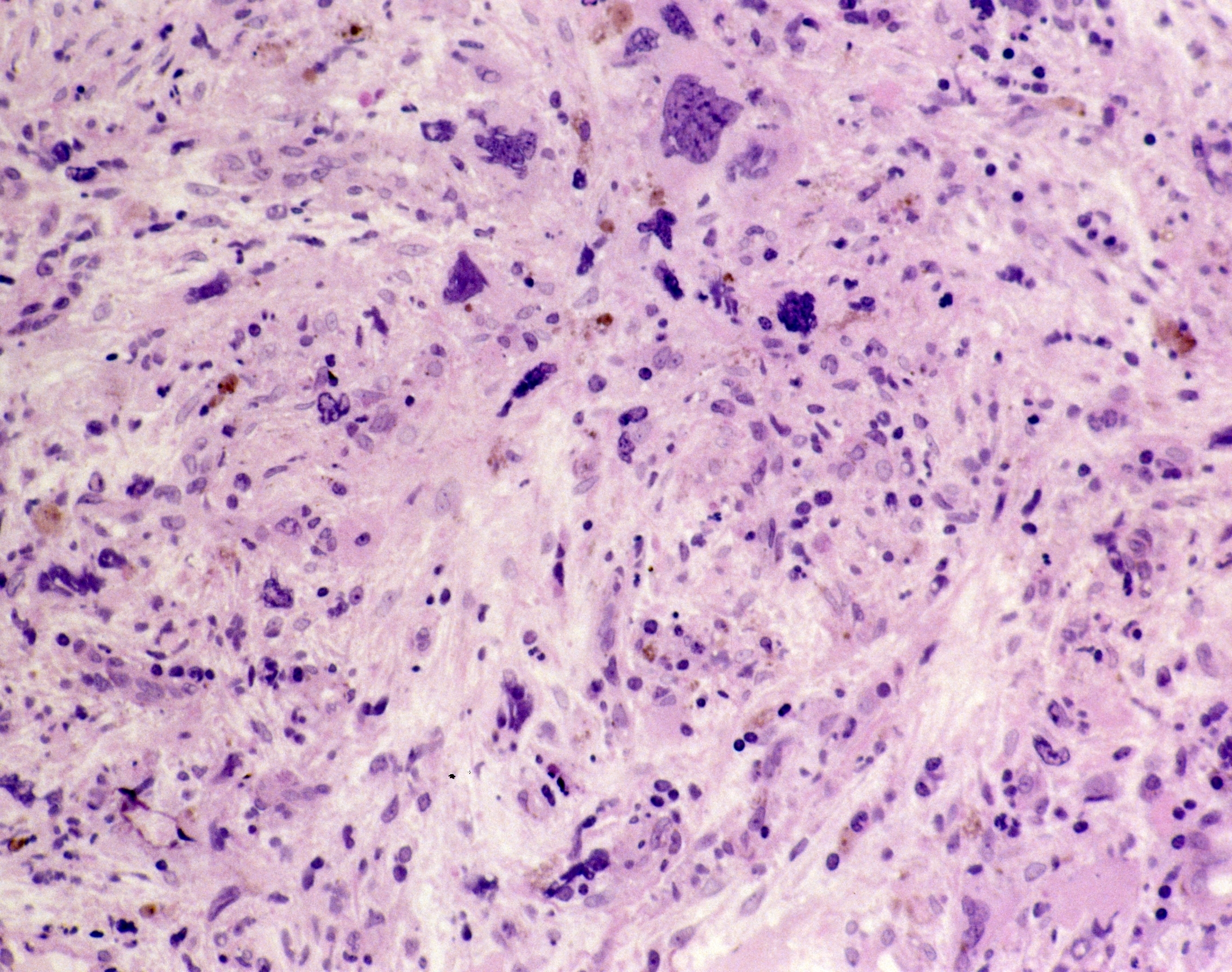
A recent case study found evidence of an acquired in utero mutation in monozygotic twins who presented with CALR mutation-positive myeloproliferative neoplasms (MPNs) with a clinical phenotype of primary myelofibrosis (MF), at ages 37 and 38 years, respectively.
This was a “remarkable case” because the mutation “originated in utero and presented with overt disease after an almost identical and prolonged latency of over 35 years in both twins,” neither of whom had a history of transfusion or other family history of MPN or another blood cancer, the authors of the case study wrote.
Nikolaos Sousos, MD, MSc, of the National Institute for Health Research Biomedical Research Centre at the University of Oxford and the Oxford University Hospitals National Health System Foundation Trust, and colleagues conducted the case study and published their findings in Nature Medicine.
The researchers determined the CALR mutation was present in myeloid cells but only at a very low level in T cells from both twins and was not detected in dermal fibroblasts from one twin, which confirmed the mutation was somatic and not present in the germline.
“In addition to CALR p.L367fs*46, which was the only shared mutation affecting a coding region, nine high-confidence [single-nucleotide variants] were also detected in both twins, strongly supporting the in utero origin of the MPN,” the researchers wrote.
Whole-genome sequencing lineage tracing determined a common clonal origin of the CALR-mutated MPN clone, “which occurred in utero followed by twin-to-twin transplacental transmission and subsequent similar disease latency,” Dr. Sousos and colleagues wrote.
An analysis of the time to the most recent common ancestor was also consistent with the mutation arising in utero. Index sorting also detected hematopoietic stem cells with the CALR mutation in both twins, suggesting the hematopoietic stem cell is the propagating cell for the MPN clone.
Due to the in utero origin of the acquired CALR mutations in the twins, the researchers analyzed neonatal blood spots from three patients with MPN who had a JAK2 V617F mutation. Of these patients, one had the mutation present in their neonatal blood spot, and this patient was diagnosed with JAK2 V617F mutation-positive polycythemia vera at age 34 years.
“These findings support that an in utero origin of the MPN clone, presenting after a prolonged disease latency, may be a widespread phenomenon in MPN, warranting further studies,” the researchers wrote.
Dr. Sousos and colleagues recommended larger genetic studies of hematologic malignancies in monozygotic twins and analysis of neonatal blood spots in patients with sporadic MPNs, as “this will provide a unique window into the evolution of MPNs and fitness advantage exerted by MPN-associated driver mutations” and may even pave the way for specific treatments aimed at patients who have mutations that arose in utero.
“Although currently the only curative treatment for MPN remains [bone marrow] transplantation, there is accumulating evidence that certain treatments such as interferon or targeted inhibitors can induce molecular remissions, and it is also possible that the fetal origin in some cases of MPN might also present unanticipated therapeutic vulnerabilities, paving the way for disease-modifying early intervention strategies,” Dr. Sousos and colleagues concluded.
Reference
Sousos N, Ní Leathlobhair M, Simoglou Karali C, et al. In utero origin of myelofibrosis presenting in adult monozygotic twins. Nat Med. 2022;28(6):1207-1211.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.