Adding navitoclax, a BCL-XL/BCL-2 inhibitor, to ruxolitinib led to durable spleen volume reductions and improved total symptom scores in patients with persistent or progressive myelofibrosis.
Claire Harrison, BMBCh, DM, FRCP, FRCPath, of Guy’s and St. Thomas’ National Health System Foundation Trust, and colleagues conducted the phase II trial because “targeting the BCL-XL pathway has demonstrated the ability to overcome Janus kinase inhibitor resistance in preclinical models.”
The open-label, multicenter trial comprised 34 adults with intermediate to high-risk myelofibrosis who had disease progression or suboptimal response while receiving a stable dose of ruxolitinib 10 mg or more twice daily. All patients additionally received navitoclax 50 mg once daily as a starting dose, escalating in weekly increments to a maximum dose of 300 mg once daily if a patient’s platelets were ≥75 × 109/L.
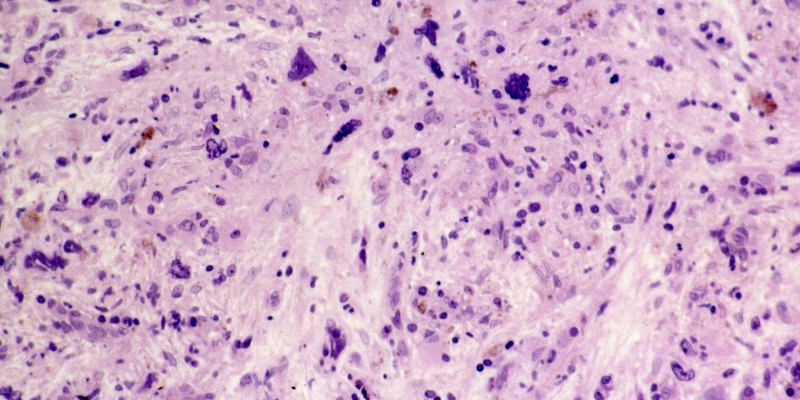
The trial’s primary endpoint was a spleen volume reduction of at least 35% from baseline to week 24. Secondary endpoints included a reduction of at least 50% in the total symptom score from baseline to week 24, change in bone marrow fibrosis grade, and safety.
More than a quarter (26.5%) of patients had a spleen volume reduction of at least 35% by week 24, while 41% of patients had a spleen volume reduction of at least 35% at any point during the study. The estimated median duration of a spleen volume reduction of at least 35% was 13.8 months (95% CI, 8.2 to not estimable).
A total symptom score reduction of at least 50% occurred in 30% of patients by week 24. The bone marrow fibrosis grade improved by one to two grades in 33% of patients who were evaluable. Most patients (64%) had an anemia response, including a patient who had baseline transfusion dependence.
The median overall survival (OS) was not reached after a median follow-up of 21.6 months, while the estimated survival at 24 months was 84% (95% CI, 63.0-93.9).
More than half (58%) of patients had high-risk mutations, with 52% harboring at least three mutations. There was no significant difference in OS between the 19 patients who had high-risk mutations and the 14 patients without high-risk mutations.
The most common adverse event was reversible thrombocytopenia without clinically significant bleeding, which occurred in 88% of patients.
The study’s findings are “potentially significant” for this population of patients, but the trial’s open-label design, small sample size, and lack of comparison group were limitations, according to the authors.
“Combining navitoclax with ongoing ruxolitinib was manageable in this difficult-to-treat population, demonstrating encouraging and durable efficacy outcomes for this patient population who have limited treatment options,” the authors concluded.
Reference
Harrison CN, Garcia JS, Somervaille TCP, et al. Addition of navitoclax to ongoing ruxolitinib therapy for patients with myelofibrosis with progression or suboptimal response: phase II safety and efficacy. J Clin Oncol. 2022;40(15):1671-1680. doi:10.1200/JCO.21.02188






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.