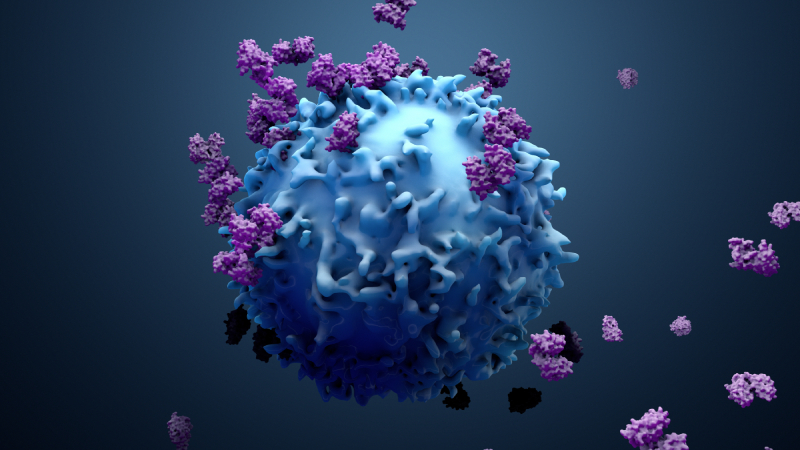
In January, the US Food and Drug Administration (FDA) notified manufacturers of both BCMA- and CD19-directed chimeric antigen receptor (CAR) T-cell therapies that it would require product safety information to include a boxed warning for T-cell malignancies.1
In a series of letters sent to the manufacturers, the FDA said it had “become aware of the risk of T-cell malignancies, with serious outcomes, including hospitalization and death, following treatment with BCMA- and CD19-directed genetically modified autologous T-cell immunotherapies.” Based on this “new safety information,” the product must henceforth carry a boxed warning reading, “T-cell malignancies have occurred following treatment with BCMA- and CD19-directed genetically modified autologous T-cell immunotherapies.”2
This action followed a November 2023 announcement that the FDA was investigating serious risk of T-cell malignancy in these CAR T-cell immunotherapies.3 Products affected include brexucabtagene autoleucel (Tecartus, Kite), idecabtagene vicleucel (ide-cel; Abecma, Bristol Myers Squibb), lisocabtagene maraleucel (Breyanzi, Bristol Myers Squibb), ciltacabtagene autoleucel (cilta-cel; Carvykti, Janssen Oncology and Legend Biotech), tisagenlecleucel (Kymriah, Novartis), and axicabtagene ciloleucel (Yescarta, Kite).1
“I am not surprised that the ‘Black Box’ warning came out based on what was reported in November,” said Damian Green, MD, Chief of the University of Miami’s Sylvester Comprehensive Cancer Center’s Division of Transplantation and Cellular Therapy, “but there are many other factors that must also be considered when we think about approaching CAR T-cell therapy in patients.”
What Are the Details?
In November 2023, the FDA issued a summary stating that it had received reports of T-cell malignancies, including a CAR-positive lymphoma, in patients who had received BCMA- or CD19-directed autologous CAR T-cell therapy. The statement revealed that the reports were from clinical trial and postmarketing adverse event data sources but did not provide more specifics.
Only limited information on these cases was available. In late 2023, news outlets reported that the FDA had received approximately 20 reports of T-cell malignancies.4,5 This report was confirmed in a New England Journal of Medicine Perspective published in February in which Nicole Verdun, MD, and Peter Marks, MD, PhD, of the FDA’s Center for Biologics Evaluation and Research, wrote that as of December 31, 2023, the FDA was aware of 22 cases of T-cell malignancies that occurred after receipt of CAR T-cell therapies.6
The cases included T-cell lymphoma, T-cell large granular lymphocytosis, peripheral T-cell lymphoma, and cutaneous T-cell lymphoma. Fourteen of the 22 cases have adequate data available; all of them occurred within two years of administration, with about half occurring within the first year.
“In three cases for which genetic sequencing has been performed to date, the CAR transgene has been detected in the malignant clone, which indicates that the CAR-T product was most likely involved in the development of the T-cell cancer,” Drs. Verdun and Marks wrote.
Simon Harrison, MBBS, PhD, Director of the Centre of Excellence for Cellular Immunotherapy and a hematologist at Peter MacCallum Cancer Centre in Victoria, Australia, told Blood Cancers Today that, as far as he is aware, his team has published details on the only CAR-positive T-cell malignancy in multiple myeloma (MM).7
An online-only abstract from the 2023 American Society of Hematology (ASH) Annual Meeting & Exposition detailed a patient enrolled in the CARTITUDE-4 study who was diagnosed with a CAR-positive T-cell lymphoma after receipt of cilta-cel, an anti-BCMA CAR-T therapy. The 51-year-old male patient achieved stringent complete response and measurable residual disease negativity. Five months after infusion, “a relatively rapidly growing erythematous nasofacial plaque developed” and a T-cell lymphoma was subsequently diagnosed, with analysis revealing that 90% to 100% of lymph node biopsy cells were CAR-positive.7
“In this case, the patient had many other things going on genetically that put him at high predisposition at the time,” Dr. Harrison said, including a germline mutation seen in T-cell malignancies.
“This rare malignancy was potentially driven by genetic mutations (eg, TET2, NFKB2, PTPRB, or JAK3), some of which may have existed in the form of a clone with malignant potential before cilta-cel manufacturing (eg, TET2 p.H1416R and JAK3 p.V722I variants),” Dr. Harrison and colleagues wrote in the abstract. “A potential contributory role of the CAR insertion in the three-inch untranslated region of PBX2 to [T-cell lymphoma] development remains unclear and cannot be excluded at this time.”
In another 2023 ASH abstract, researchers from China detailed outcomes from 48 patients with relapsed or refractory B-cell non-Hodgkin lymphoma treated with C-CAR039, an autologous anti-CD20/CD19 bispecific CAR T-cell therapy. Researchers observed secondary primary malignancies in three patients, one of which was an Epstein-Barr virus–positive, cytotoxic T-cell lymphoma at eight months after C-CAR039 infusion. None was related to C-CAR039.8
In January, researchers from the University of Pennsylvania published details of a retrospective study of 449 patients treated with CAR T-cell therapy at Penn Medicine and found with a median follow-up of 10.3 months that only 3.6% of patients had a secondary primary malignancy. They found only a single case of an incidental T-cell lymphoma that did not express the CAR gene; this lymphoma was found in a patient who had developed a secondary lung tumor after CAR T-cell therapy.9
More Information Needed
The recognition of a possible risk for T-cell malignancies related to gene therapy has long been recognized, according to Sergio Giralt, MD, Chief of Adult Bone Marrow Transplant at Memorial Sloan Kettering Cancer Center.
“We all recognize that with all genetically modified treatments, or with genetically modified cells, there is a possibility that you could potentially introduce oncogenic stimuli into normal cells and potentially make malignant cells more malignant,” Dr. Giralt said. “That is why these cellular therapies like CAR T-cell therapy undergo rigorous and extensive clinical trials before they become commercially available.”
Dr. Green said that he recognized the FDA is requiring these warnings in an attempt to protect the public, but he added that there is currently no quantification of the risk.
Dr. Giralt agreed. “Is the risk one in a million? Is it one in 1,000? We don’t know.” The FDA has still not provided much information on the exact characteristics of each of these cases. He said that his institution’s dataset reveals second primary malignancies after CAR T-cell therapy but no T-cell malignancies.
“As clinicians and the people involved in the development of these products, the real-world incidence [of T-cell malignancies] has been very low based on available data up to this juncture,” Dr. Green said. “These warnings don’t substantially change how we think about approaching CAR T-cell therapy in our patients.”
Clinicians are still trying to understand the cause of the T-cell malignancies. Is it CAR-T or something else?
“One question that someone posed (where T-cell malignancies are concerned) is whether they are related to the CAR T-cell therapy or to significant immune deficiency that patients have because they are extensively pretreated with therapies that inhibit their immune system,” Dr. Giralt said.
Dr. Harrison echoed this possibility, pointing out that therapies such as fludarabine, which modulate the composition and function of T cells, also have signals for myeloid malignancies.10
“People are looking at this more carefully, particularly in relation to cilta-cell,” Dr. Harrison said. The original LEGEND-2 trial of cilta-cell used lymphodepleting chemotherapy with cyclophosphamide only, but “fludarabine was added because it became the standard in the field,” he noted.
The addition of fludarabine to cyclophosphamide improved outcomes related to CD19 CAR T-cell therapy.11 However, fludarabine was found to be associated with increased toxicities in patients with relapsed or refractory MM treated with ide-cel,12 and national shortages of the drug have led to analysis of alternative lymphodepletion regimens that may be equally effective.13
“Fludarabine made a difference in CD19 land, but does it still need to be there in cilta-cel land?” Dr. Harrison said. “That study probably needs to be done in terms of changing lymphodepletion and asking if we still need [fludarabine].”
Patient Conversations
Patients are aware of these FDA warnings, according to Dr. Harrison, especially the ones who are more informed.
“Conversations typically revolve more around the acute toxicities,” he said. “In myeloma, long-term survivors get second malignancies. We know that.”
These patients get melphalan, immunomodulatory agents, cyclophosphamide … they get [secondary] malignancies, Dr. Harrison noted. That is not new information.
Dr. Giralt said that with increased awareness of this guidance from the FDA, he informs patients that there have been cases of T-cell malignancies reported after CAR T-cell therapies.
“I tell them that the potential benefit still far outweighs the risk,” he said. “The main reason that people die after CAR T-cell therapy is their malignancy. People don’t respond to treatment or have rare toxicities related to infections or because their immune system is affected.”
In an editorial in Blood Advances last year, Rahul Banerjee, MD, of the University of Washington, and colleagues suggested the use of a three-pronged approach when addressing patient concerns about the possibility of T-cell malignancies.14
First, emphasize that the benefits of CAR T-cell therapy far outweigh the risks, a statement backed up by the FDA.
“As clinicians and research scientists, our job is to do what we feel is most likely to be in the patient’s best interest with respect to both quantity and quality of life,” Dr. Green said. “We weigh the risks for second cancers in many settings, including stem cell transplant, chemotherapeutic and radiation therapies.”
Second, explain that several factors other than the CAR T-cell therapy itself could explain why certain patients developed second primary malignancies, including treatments undertaken prior to CAR-T.
“Patients can only develop second primary malignancies if they do not first die of their primary malignancies; as such, patients who receive effective cancer therapies will have higher rates of second primary malignancies compared [with] patients who do not,” Dr. Banerjee and colleagues wrote.
Third, the active cancer is a greater risk than the hypothetical risk of a future cancer.
“If the patient succumbs to their current cancer, it is a moot point if there is a risk for secondary cancer,” Dr. Green said. “I don’t want to minimize the risk, but you would be hard-pressed to find a patient who would say ‘Don’t give me a therapy that is likely to prolong my life’ out of concern that at some point in the future it might, perhaps slightly, increase risk for a second cancer.”
Future Effects
Experts agreed that these new “Black Box” warnings are unlikely to have a significant effect on these therapies going forward, but some changes are possible. One possible effect is delaying CAR T-cell therapy until later lines of treatment where possible, Dr. Giralt said.
“Patients may have an alternative treatment with the use of bispecific antibodies, particularly in myeloma,” he noted. “That may lead to some patients choosing a bispecific before the CAR-T because of risk of cancer.” However, he added that bispecifics are not without their own risks.
Dr. Green said that previously there was a mandate to follow patients undergoing CAR T-cell therapy for 15 years. Now, patients should likely be followed for the rest of their lives.
“When patients enroll in clinical trials, it is their prerogative to decide how long they want to participate in follow-up,” Dr. Green said. “We should emphasize the importance of working in partnership with patients to hopefully encourage them to stay involved and allow us to follow them over the arc of their experience so we can identify any problems arising.”
Despite the FDA’s action, the Australia Therapeutic Goods Administration has not yet issued a response; CAR T-cell therapy is not approved in Australia and only administered as part of clinical trials. In January, the European Medicines Agency announced it would begin to review data on secondary malignancies seen after CAR T-cell therapies.15 In the end, what is needed is time, Dr. Harrison said.
“Accumulating numbers is the only way to be clear one way or another if there is an excess of T-cell malignancies or not,” he noted. “There is an inherent bias in positive reporting at the moment, and time will help determine if this is just background noise or if it is the real thing.”
Once it is determined if the risk is real, Dr. Harrison said, the field can look at the numbers and decide if the amount of risk is acceptable.
Leah Lawrence is a freelance health writer and editor based in Delaware.
References
- 2024 safety and availability communications. FDA. January 2024. Accessed March 1, 2024. https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/2024-safety-and-availability-communications
- Verdun N. Safety labeling change notification letter – ABECMA (idecabtagene vicleucel). FDA. January 19, 2024. Accessed March 1, 2024. https://www.fda.gov/media/175623/download?attachment
- FDA investigating serious risk of T-cell malignancy following BCMA-directed or CD19-directed autologous chimeric antigen receptor (CAR) T cell immunotherapies. FDA. November 28, 2023. Accessed March 1, 2024. https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/fda-investigating-serious-risk-t-cell-malignancy-following-bcma-directed-or-cd19-directed-autologous
- Chen A. Blood cancers may arise from CAR-T cells, but experts think only in very rare cases. STAT. November 29, 2023. Accessed April 1, 2024. https://www.statnews.com/2023/11/29/blood-cancer-car-t-therapy-fda-investigation/
- Erman M, Beasley D. US FDA examined 22 cases of cancers in CAR-T probe -officials. Reuters. January 24, 2024. Accessed April 1, 2024. https://www.reuters.com/business/healthcare-pharmaceuticals/us-fda-examined-22-cases-cancers-car-t-probe-officials-2024-01-24/
- Verdun N, Marks P. Secondary cancers after chimeric antigen receptor T-cell therapy. N Engl J Med. 2024;390(7):584-586. doi:10.1056/NEJMp2400209
- Harrison SJ, Nguyen T, Rahman M, et al. CAR+ T-cell lymphoma post ciltacabtagene autoleucel therapy for relapsed refractory multiple myeloma. Blood. 2023;142(Supplement 1):6939. doi:10.1182/blood-2023-178806
- Li P, Yu W-J, Zhou L, et al. C-CAR039, a novel anti-CD20/CD19 bi-specific CAR T-cell therapy shows deep and durable clinical benefits in patients with relapsed or refractory (r/r) B-cell non-Hodgkin lymphoma (B-NHL) in long term follow up. Blood. 2023;142(Supplement 1):1025. doi:10.1182/blood-2023-182817
- Ghilardi G, Fraietta JA, Gerson JN, et al. T cell lymphoma and secondary primary malignancy risk after commercial CAR T cell therapy. Nat Med. 2024. doi:10.1038/s41591-024-02826-w
- Laribi K, de Materre AB, Ghez D, et al. Therapy-related myeloid neoplasms in patients with chronic lymphocytic leukemia who received FCR/FC as frontline therapy. Hemasphere. 2022. doi:10.1097/HS9.0000000000000716
- Dekker L, Calkoen FG, Jiang Y, et al. Fludarabine exposure predicts outcome after CD19 CAR T-cell therapy in children and young adults with acute leukemia. Blood Adv. 2022;6(7):1969-1976. doi:10.1182/bloodadvances.2021006700
- Wagner CB, Sweiss K, Anto E, et al. Fludarabine lymphodepletion exposure is associated with idecabtagene vicleucel toxicity in relapsed and refractory multiple myeloma patients: real-world experience from the US Myeloma Immunotherapy Consortium. Blood. 2023;142(Supplement 1): 4880. doi:10.1182/blood-2023-187440
- Gill SK, Biran N, Phull P, et al. Comparison of fludarabine/cyclophosphamide vs bendamustine as lymphodepleting regimen for CAR-T: a safety and efficacy analysis in patients with relapsed/refractory multiple myeloma. Blood. 2023;142(Supplement 1):6903. doi:0.1182/blood-2023-190507
- Banerjee R, Poh C, Hirayama AV, et al. Answering the “doctor, can CAR-T therapy cause cancer?” question in clinic. Blood Adv. 2024;8(4):895-898. doi:10.1182/bloodadvances.2023012336
- Meeting highlights from the Pharmacovigilance Risk Assessment Committee (PRAC) 8-11 January 2024. European Medicines Agency. January 12, 2024. Accessed March 5, 2024. https://www.ema.europa.eu/en/news/meeting-highlights-pharmacovigilance-risk-assessment-committee-prac-8-11-january-2024



 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.