
Take-aways:
- From 1974 to 2014, rates of late mortality after ASCT have decreased, but the reduction was specific to younger patients or those who received a bone marrow transplant.
- Life expectancy has improved since 1974 but remains 20.8% lower compared with the general population.
- Further efforts to mitigate disease recurrence, infections, subsequent neoplasms, cardiovascular disease, and pulmonary disease may be useful in this population.
Over the past 40 years, the risks of late mortality after allogeneic stem cell transplantation (ASCT) have decreased substantially, with patients gaining approximately 5 years in life expectancy, according to results from a cohort study published in JAMA Oncology.
However, study authors, led by Smita Bhatia, MD, MPH, from the University of Alabama at Birmingham, reported that the observed reductions in late mortality were specific to patients who underwent ASCT at a young age or received transplant with bone marrow as opposed to peripheral blood.
ASCT with hematopoietic stem cells derived from donor peripheral blood or bone marrow represents a potentially curative option for patients with high-risk or relapsed hematologic malignancies, but the procedure is associated with higher risks of morbidity and mortality in the years following.
“The past 4 decades have seen substantial changes in allogeneic blood or marrow transplantation practice, with the overarching goal of expanding the eligible patient pool while optimizing disease-free survival,” Dr. Bhatia and colleagues wrote.
In this study, the researchers conducted a retrospective cohort study of 4,741 individuals who lived 2 or more years after ASCT performed between January 1, 1974, and December 31, 2014. Outcomes were analyzed according to ASCT performed in 3 eras: 1974 to 1989, 1990 to 2004, and 2005 to 2014. Study authors evaluated all-cause, recurrence-related, and nonrecurrence-related mortality and projected reduction in life expectancy. Information regarding vital status and cause of death was obtained from the National Death Index Plus and Accurint databases.
The median age at ASCT in the cohort was 33 years (range, 0-75). The cumulative incidence of recurrence-related mortality appeared to plateau at 10 years, with cumulative incidence reaching 12.2% at 30 years after ASCT. In contrast, the incidence of nonrecurrence-related mortality continued to increase and was 22.3% at 30 years.
The leading causes of nonrecurrence-related mortality included infection, subsequent malignant neoplasms, cardiovascular disease, and pulmonary disease (Table 1).
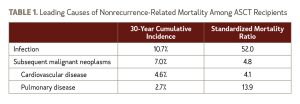
Compared with the general population, the relative mortality among ASCT recipients remained higher at 30 or more years after transplant, with a standardized mortality ratio (SMR) of 5.4. Overall, the ASCT cohort experienced a 20.8% reduction in life expectancy, equivalent to 8.7 years of life lost.
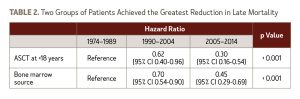
Compared with the reference period of 1974-1989, the adjusted 10-year hazard ratio (HR) for all-cause mortality declined over the 3 eras (HR, 0.67 for 1990-2004 and HR, 0.52 for 2005-2014; P < .001).
Life expectancy post-ASCT continually improved in each era analyzed, with fewer years of life lost between 1974 and 2014:
- 1974-1989: 9.9 years
- 1990-2004: 6.5 years
- 2005-2014: 4.2 years
Dr. Bhatia and colleagues noted that the reduction in late mortality was most pronounced among individuals who underwent ASCT as children (<18 years) and those who received bone marrow transplant (Table 2).
Given that older patients or those who received peripheral blood transplant did not experience any meaningful decline in late mortality, “further efforts to mitigate disease recurrence, infections, subsequent neoplasms, cardiovascular disease, and pulmonary disease may be useful in this population,” the authors concluded.
Disclosures: The study authors reported no relevant conflicts of interest.
Reference
Bhatia S, Dai C, Landler W, et al. Trends in late mortality and life expectancy after allogeneic blood or marrow transplantation over 4 decades: a Blood or Marrow Transplant Survivor Study report. JAMA Onc. 2021;7(11):1626-1634.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.