Take-aways:
- Lenalidomide plus rituximab led to a similar ORR, PFS, and CR rate compared with rituximab plus chemotherapy in patients with previously untreated advanced-stage follicular lymphoma.
- Patients in the two treatment groups had similar rates of progression and relapse.
- The doublet treatment and rituximab plus chemotherapy showed comparable safety and efficacy after six years of follow-up.
Lenalidomide plus rituximab is “an acceptable chemotherapy-free alternative” to rituximab plus chemotherapy in patients with previously untreated advanced-stage follicular lymphoma (FL), according to long-term results from the phase III RELEVANCE trial.
While immunochemotherapy has “remained the frontline gold standard for patients with FL needing systemic therapy,” Franck Morschhauser, MD, PhD, of University of Lille’s Centre Hospitalier Universitaire de Lille in France, and colleagues conducted the RELEVANCE trial because FL can be “immune-responsive to non-chemotherapy regimens.”
For example, combining the immunomodulator lenalidomide with rituximab, an anti-CD20 monoclonal antibody, showed “promising activity with high response rates” in patients with previously untreated FL in previous phase II trials, according to Dr. Morschhauser and colleagues.
Earlier results from the RELEVANCE trial showed lenalidomide plus rituximab “provided similar efficacy” to rituximab plus chemotherapy, but the researchers conducted the six-year follow-up analysis because long-term data on the toxicity and efficacy of the doublet treatment are “highly needed,” they wrote.
Study Design and Methods
The RELEVANCE investigators randomly assigned patients 1:1 to receive lenalidomide plus rituximab (n=513) or rituximab plus chemotherapy followed by rituximab maintenance (n=517). For patients receiving rituximab plus chemotherapy, the investigators chose among chemotherapy regimens of cyclophosphamide, doxorubicin, vincristine, and prednisone (n=28); bendamustine (n=117); or cyclophosphamide, vincristine, and prednisone (n=372).
Nearly all patients receiving lenalidomide plus rituximab (99%) received at least one dose of the study drug, with 69% completing the full 120 weeks of treatment. The same was true for patients receiving rituximab plus chemotherapy, as 97% received at least one dose of the study drug, and 71% completed the full course of treatment. Most patients receiving rituximab plus lenalidomide (81.7%) and most patients receiving rituximab plus chemotherapy (77.4%) entered clinical follow-up.
The study’s co-primary endpoints were the confirmed/unconfirmed complete response (CR) rate at 120 weeks and PFS as assessed by an Independent Review Committee per 1999 International Working Group criteria. The researchers also conducted post hoc exploratory analyses on survival from a risk-defining event according to progression of disease within two years of first-line therapy.
Results
The overall response rate (ORR) was similar between treatment groups: 61% in patients receiving the doublet and 65% in those receiving rituximab plus chemotherapy. Confirmed/unconfirmed CR rates were also similar between groups: 48% in patients receiving the doublet and 53% in those receiving rituximab plus chemotherapy (P=.10). See TABLE 1 for a summary of responses.
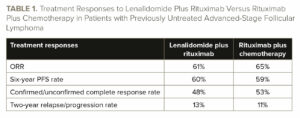
PFS was also similar between groups (hazard ratio, 1.03; 95% CI, 0.84-1.27; P=.78), with a six-year PFS rate of 60% (95% CI, 55-64) in patients receiving the doublet and 59% (95% CI, 54-64) in patients receiving rituximab plus chemotherapy. The median PFS was not reached in either group after a median follow-up of 72 months and 354 PFS events.
“Subgroup analyses of PFS were consistent with the first interim analysis,” Dr. Morschhauser and colleagues wrote. “The efficacy of [lenalidomide plus rituximab] continued to be independent of conventional prognostic factors, including disease stage, Follicular Lymphoma International Prognostic Index score, bulky disease, and age.”
The researchers estimated the six-year OS rate was 89% in both treatment groups. The median OS was not reached in either group.
“Similarly, event-free survival and time to next anti-lymphoma treatment did not differ significantly between the groups,” Dr. Morchhauser and colleagues wrote. “Exploratory analysis on the three different [rituximab plus] chemotherapy groups showed no statistical difference in PFS, by [Independent Review Committee] and investigator, nor OS.”
The rate of relapse or progression within the first two years of first-line therapy was 13% in patients receiving the doublet and 11% in those receiving rituximab plus chemotherapy.
Progression of disease within two years of first-line therapy was associated with a significantly lower five-year survival rate of 59.5% (95% CI, 49.9-67.8) compared with the reference group’s five-year survival rate of 95.2% (95% CI, 93.3-96.6; P<.0001). However, the five-year survival rate was similar between treatment groups among patients who had disease progression, with a rate of 59% in patients receiving the doublet and 60% in those receiving rituximab plus chemotherapy.
Around a fifth of patients in each group received additional treatment after relapse. Among patients who relapsed and received additional treatment, the ORR was 61% in those who initially received the doublet treatment and 59% in those who initially received rituximab plus chemotherapy.
The confirmed/unconfirmed CR rates in patients who received additional treatment after relapse were similar between groups. The rate was 37% in patients receiving the doublet and was 45% in those receiving rituximab plus chemotherapy. There was no significant difference in survival after progression between the treatment groups.
A small fraction of patients in each treatment group had histologic transformation over a 72-month follow-up period, with a 4.4% six-year cumulative incidence of transformation in patients receiving the doublet and 3.3% in those receiving rituximab plus chemotherapy.
Secondary primary malignancies were reported in 7% of patients receiving the doublet and 10% of patients receiving rituximab plus chemotherapy in the initial analysis, increasing to 11% and 13%, respectively, in the most recent analysis.
There were slight increases in patients reporting at least one grade 5 treatment-emergent adverse event between the initial analysis and the most recent analysis, growing from six to nine patients in the group receiving the doublet and remaining stable at six patients in the group receiving rituximab plus chemotherapy.
Around one-third of patients in both the doublet and rituximab plus chemotherapy groups prematurely discontinued treatment, with progressive disease (12.5% vs 13.7%) and toxicity (8.5% vs 3.1%) being the most common reasons. Approximately one-fifth of patients in each treatment group prematurely discontinued study participation, with the most common reasons being death (54% vs 49%) and withdrawal of consent (27% vs 40%).
Deaths nearly doubled between the initial analysis and the most recent analysis, increasing from 66 to 114 deaths. Deaths occurred in 12% of patients who received the doublet and in 11% of those receiving rituximab plus chemotherapy, with eight total deaths occurring on treatment. Lymphoma caused 29 deaths in the group receiving the doublet and 17 deaths in the group receiving rituximab plus chemotherapy. Death from other causes was more common in patients receiving rituximab plus chemotherapy, occurring in 13 patients compared with six patients in the doublet group. Death from cardiac disorders occurred in four patients receiving the rituximab plus chemotherapy treatment and in no patients receiving the doublet.
“The overall safety profile in both groups was consistent with the first interim analysis, and no new safety signals were detected,” the researchers wrote.
Conclusions and Future Directions
Patients in both treatment groups “maintained very favorable outcomes” and had “excellent” six-year OS rates of 89%, according to the researchers.
Overall, the long-term results from the study showed lenalidomide plus rituximab “provides an acceptable, long-term, chemotherapy-free alternative to [rituximab plus] chemotherapy on the basis of immunomodulation in patients with advanced untreated FL in need of treatment,” Dr. Morschhauser and colleagues concluded.
The research was supported by Celgene, a Bristol Myers Squibb Company, and the Lymphoma Academic Research Organization.
Reference
Morschhauser F, Nastoupil L, Feugier P, et al. Six-year results from RELEVANCE: lenalidomide plus rituximab (R2) versus rituximab-chemotherapy followed by rituximab maintenance in untreated advanced follicular lymphoma. J Clin Oncol. 2022;40(28):3239-3245.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.