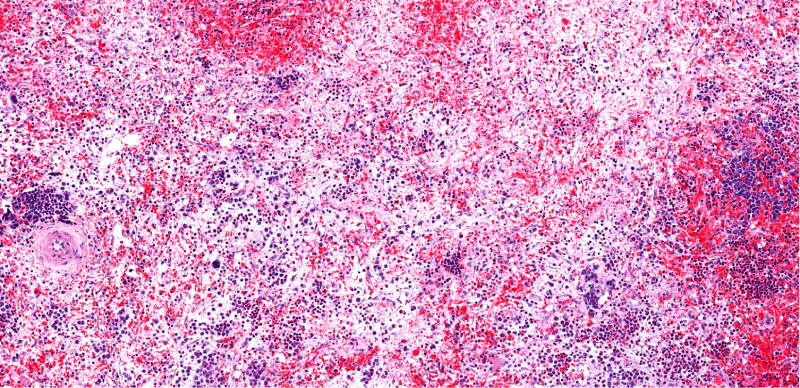
Momelotinib led to “superior” symptom and spleen responses and transfusion independence rates compared to danazol in patients with thrombocytopenic myelofibrosis who were previously treated with a Janus kinase (JAK) inhibitor, according to results from the phase III MOMENTUM study.
Aaron Gerds, MD, of the Cleveland Clinic Taussig Cancer Center, and colleagues, presented results from the MOMENTUM study at the 14th International Congress on Myeloproliferative Neoplasms.
The research follows the SIMPLIFY trials, in which momelotinib, an oral JAK1/2 and ACVR1/ALK2 inhibitor, “showed clinical activity” on myelofibrosis symptoms, red blood cell transfusion requirements, and spleen volume, including in patients with thrombocytopenia, according to Dr. Gerds and colleagues.
The researchers randomized patients 2:1 to receive momelotinib 200 mg daily plus danazol placebo, or danazol 600 mg daily plus momelotinib placebo for 24 weeks. Of the 81 patients assigned to receive momelotinib, 60 patients with baseline platelet counts of ≤150 x 109/L completed the 24-week randomized treatment phase, while 25 of the 43 patients with baseline platelet counts of ≤150 x 109/L who received danazol completed the randomized treatment phase.
The study’s primary endpoint was rate of total symptom score reductions of at least 50% from baseline to week 24. Secondary endpoints included red blood cell transfusion independence rate, splenic response rate, change from baseline in total symptom score, and rate of zero transfusions since baseline.
The median baseline total symptom score was 29 in patients treated with momelotinib and was 24 in patients treated with danazol. The total symptom score response rate at 24 weeks was greater in patients treated with momelotinib (29.6%) than in patients treated with danazol (11.6%). Patients treated with momelotinib also had a larger reduction in their total symptom score at week 24 (−10.7) than those treated with danazol (−3.8).
Patients treated with momelotinib had a higher rate of transfusion independence (32.1%) and a higher rate of no transfusions (30.9%) at week 24 than patients treated with danazol (18.6% and 11.6%, respectively).
More patients treated with momelotinib had at least a 25% reduction in spleen volume from baseline (39.5%) and at least a 35% reduction in spleen volume from baseline (22.2%) at week 24 than patients treated with danazol (7% and 4.7%, respectively).
There was a “trend toward improved” overall survival up to week 24 in patients treated with momelotinib, according to Dr. Gerds and colleagues. Additional analyses of patients with baseline platelet counts of <100 x 109/L (n=100) and <50 x 109/L (n=31) showed “similar treatment effects” with momelotinib and danazol, they reported.
The most common grade 3 or higher treatment-emergent adverse events were thrombocytopenia and anemia. Thrombocytopenia occurred in 31% of patients treated with momelotinib and in 16% treated with danazol. Anemia occurred in 7% of patients treated with momelotinib and in 14% treated with danazol.
Grade 3 or higher bleeding events occurred in 9% of patients treated with momelotinib and in 5% of patients treated with danazol. Treatment-emergent adverse events led to study drug discontinuation in 15% of patients treated with momelotinib and in 19% treated with danazol.
“Overall, in thrombocytopenic patients [with myelofibrosis] who were symptomatic and anemic, [momelotinib] was superior to [danazol] for symptom responses, transfusion requirements, and spleen responses and showed comparable safety and favorable survival,” Dr. Gerds and colleagues concluded. “[Momelotinib] may address a critical unmet need in thrombocytopenic patients [with myelofibrosis].”
Reference
Gerd A, Verstovsek S, Vannucchi A, et al. Thrombocytopenic myelofibrosis (MF) patients previously treated with a JAK inhibitor in a phase 3 randomized study of momelotinib (MMB) versus danazol (DAN) [MOMENTUM]. Presented at the 14th International Congress on Myeloproliferative Neoplasms. Abstract #117. October 27-28, 2002.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.