Take-aways:
- Event-free survival was significantly longer in patients treated with ivosidenib plus azacitidine compared with placebo plus azacitidine.
- More than half of patients with available data in the ivosidenib plus azacitidine group had IDH1 mutation clearance following treatment.
- The addition of ivosidenib to azacitidine did not significantly impact treatment-related adverse events compared with azacitidine alone.
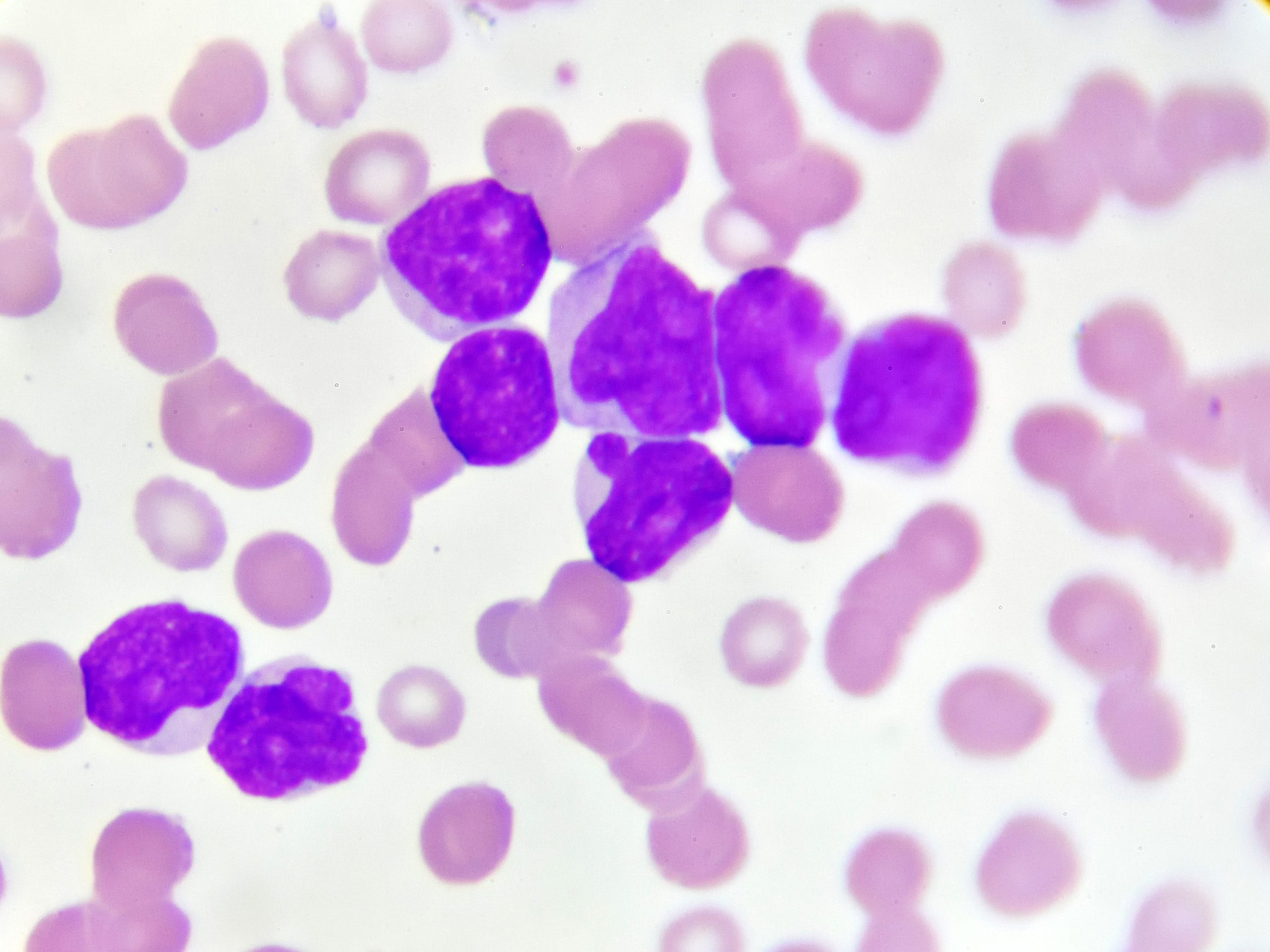
A phase III study found that combining ivosidenib and azacitidine extended event-free survival (EFS) and overall survival (OS) in IDH1-mutated acute myeloid leukemia (AML) and had similar treatment discontinuations and adverse events compared with azacitidine plus placebo.
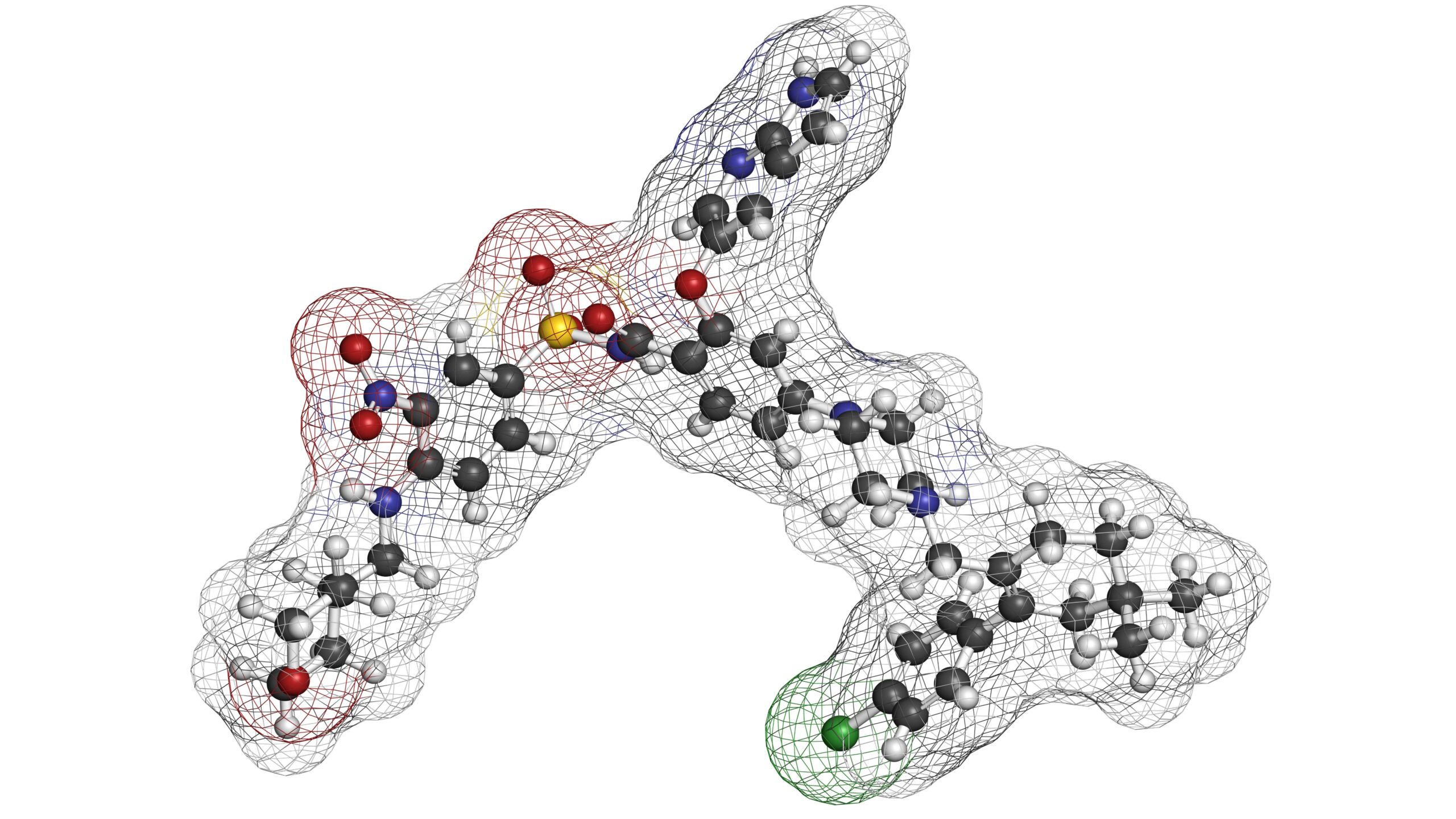
Ivosidenib is a first-in-class, oral, targeted small-molecule inhibitor of IDH1 that is approved by the U.S. Food and Drug Administration (FDA) for relapsed/refractory IDH1-mutated AML or newly diagnosed IDH1-mutated AML in patients who are 75 years or older or those who have conditions that preclude intensive chemotherapy. A prior phase Ib study of 23 patients with newly diagnosed IDH1-mutated AML showed encouraging clinical activity with ivosidenib plus azacitidine.
The recently reported global, double-blind, randomized, placebo-controlled, phase III AGILE trial assessed the safety and efficacy of ivosidenib plus azacitidine compared with placebo plus azacitidine in patients with newly diagnosed IDH1-mutated AML who were ineligible for intensive induction chemotherapy. The results of the trial were published in The New England Journal of Medicine by Pau Montesinos, MD, PhD, of the University Hospital La Fe in Valencia, Spain, and coauthors.
Adult patients were eligible if they had a centrally confirmed diagnosis of previously untreated IDH1-mutated AML as determined by the FDA-approved Abbott RealTime IDH1 in vitro polymerase chain reaction assay, received no prior treatment with an IDH1 inhibitor or hypomethylating agent for myelodysplastic syndromes, had an Eastern Cooperative Oncology Group performance status score of 0-2, and had adequate hepatic and renal function. Patients with a severe cardiac or pulmonary disorder, creatinine clearance of <45 mL/min, or a bilirubin level >1.5 times the upper limit of normal were excluded.
Patients (n=146) were enrolled between March 2018 and May 2021 and received azacitidine 75 mg/m2 subcutaneously or intravenously for seven days of each 28-day cycle and were randomized 1:1 to receive ivosidenib 500 mg administered orally daily (n=72) or placebo (n=74). All patients continued treatment for a minimum of six treatment cycles or until relapse, disease progression, unacceptable toxicity, or death.
At data cutoff, 39 patients were still receiving treatment: 27 (38%) in the ivosidenib plus azacitidine group and 12 (16%) in the placebo plus azacitidine group.
Primary and secondary efficacy outcomes
After a median of 12.4 months of follow-up, EFS (primary endpoint) was significantly longer in the ivosidenib plus azacitidine group compared with placebo plus azacitidine (hazard ratio [HR] for treatment failure, relapse from remission, or death=0.33; 95% CI, 0.16-0.69; P=.002). Less than half of patients in each treatment cohort had complete remission by week 24, so the median EFS was the same: 0.03 months. However, estimated probability of 12-month EFS was 37% in the ivosidenib plus azacitidine group versus 12% in the placebo plus azacitidine cohort.
A total of 74 deaths occurred: 28 (39%) in the ivosidenib plus azacitidine group and 46 (62%) in the placebo plus azacitidine cohort. Median OS (secondary endpoint) was 24.0 months in the ivosidenib plus azacitidine group versus 7.9 months with placebo plus azacitidine (HR for death=0.44; 95% CI 0.27-0.73; P=.001).
Complete remission occurred in 34 patients (47%) in the ivosidenib plus azacitidine group and 11 (15%) in the placebo plus azacitidine group, with the median duration of complete remission not reached in the ivosidenib plus azacitidine cohort and 11.2 months in the placebo plus azacitidine group. Median time to complete remission was 4.3 months (range, 1.7-9.2 months) and 3.8 months (range, 1.9-8.5 months), respectively.
Median treatment duration was 6.0 months (range, 0.1-33.5 months) with ivosidenib plus azacitidine versus 2.8 months (range, 0.1-19.8 months) with placebo plus azacitidine.
Among patients who were transfusion-dependent of red blood cells, platelets, or both at baseline, 46% of patients in the ivosidenib plus azacitidine group were transfusion-independent after treatment compared with 18% of placebo plus azacitidine-treated patients (P=.006).
IDH1 mutation clearance (defined as non-detection of IDH1 mutation at one or more time points during study treatment) was assessed in bone marrow mononuclear cells. Among patients with available samples, 52% of patients (n=17/33) in the ivosidenib plus azacitidine group had IDH1 mutation clearance versus 30% (n=3/10) in the placebo plus azacitidine group. Among those who had IDH1 mutation clearance, 33% (n=14/43) had complete remission with IDH1 mutation clearance in the ivosidenib plus azacitidine group compared with 6% (n=2/31) in the placebo cohort (P=.009). The researchers said these results “highlight the benefit of targeting the mutant IDH1 protein.”
Safety data
Grade ≥3 adverse events were reported in 66 patients (93%) receiving ivosidenib plus azacitidine and 69 patients (95%) in the placebo plus azacitidine cohort. The most common grade ≥3 adverse events in the ivosidenib plus azacitidine and placebo plus azacitidine groups were febrile neutropenia (28% vs 34%, respectively), anemia (25% vs 26%, respectively), neutropenia (27% vs 16%, respectively), thrombocytopenia (24% vs 21%, respectively), and pneumonia (23% vs 29%, respectively).
The incidence of any-grade infection was 28% with ivosidenib plus azacitidine and 49% with placebo plus azacitidine. Only the ivosidenib plus azacitidine group experienced increased absolute neutrophil counts from baseline. Bleeding events were also more common in the ivosidenib plus azacitidine cohort (41% vs 29%). Nineteen patients in each cohort discontinued treatment due to adverse events, and 4 patients (6%) in the ivosidenib plus azacitidine group required dose reductions due to adverse events.
Fewer patients were recruited to the trial than initially planned, according to the authors, which limits the data interpretation in some preplanned subgroup analyses. Another limitation of the study is the use of EFS as the primary endpoint rather than the gold-standard OS.
“Because this trial showed a robust improvement in all efficacy endpoints, it becomes important to consider the positioning of this new option in the current treatment landscape, which includes venetoclax-based regimens,” the authors wrote of their findings. “Future studies comparing venetoclax-based treatment with ivosidenib and azacitidine or evaluating the combination of these regimens would be of interest.”
Disclosures: This research was supported by Agios Pharmaceuticals and Servier Pharmaceuticals, which acquired Agios’ oncology business and is the manufacturer of ivosidenib.
Reference
Montesinos P, Recher C, Vives S, et al. Ivosidenib and azacitidine in IDH1-mutated acute myeloid leukemia. N Engl J Med. 2022;386(16):1519-1531.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.