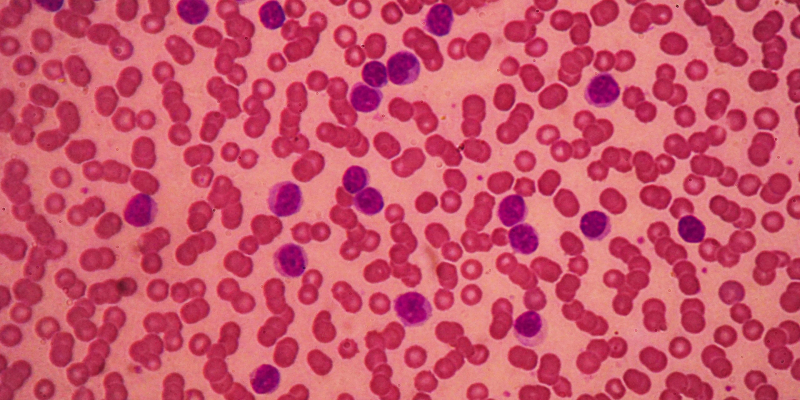
A new study has identified two proteolysis targeting chimeras—or PROTACs—that may help overcome venetoclax-resistant chronic lymphocytic leukemia (CLL) dependent on BCL-xL and mutant BCL2.
Daisy Diaz Rohena, BS, of the University of Texas MD Anderson Cancer Center in Houston, presented an abstract at the 65th ASH Annual Meeting and Exposition detailing an analysis that used single-cell RNA sequencing of paired samples from a CLL patient collected at baseline and again at relapse. Relapse had occurred after cessation of fixed-duration treatment with the BCL2-targeting venetoclax and BTK-targeting ibrutinib.
The researchers found that the proportion of cells in each CLL cluster was vastly different at relapse than it was at baseline. For example, cluster 3 represented 4% of CLL cells at baseline compared with 36% at relapse. Additionally, the sample at relapse had more CLL cells expressing transcripts from the BCL2 family of proteins, including BCL2 and BCL-xL.
Next, the researchers tested BCL2/BCL-xL–targeting PROTACs PZ18753b and WH25244—both derived from navitoclax—in three models of venetoclax-resistant CLL. They found that WH25244 was superior to venetoclax at targeting OSU-CLL cells expressing wild-type or mutant BCL2. Additionally, cell death by WH25244 was preceded by degradation of BCL-xL and partial degradation of BCL2.
In treatment-naïve CLL cells, degradation by both PROTACs proceeded in a dose-, time-, and von Hippel-Lindau-dependent manner, the researchers wrote.
They concluded: “Relative to its precursor, navitoclax, it shows increased potency against CLL cells and decreased toxicity against platelets in vitro, due to its VHL-dependent activity and minimal expression of VHL in platelets.”
Reference
Rohena DD, Cuesta AP, Slawin B, et al. Enriched signaling pathways in venetoclax-relapsed chronic lymphocytic leukemia (CLL) cells and targeting using a PROTAC-based BCL-2/BCL-xL degrader. Abstract #4195. Presented at the 65th ASH Annual Meeting and Exposition; December 9-12, 2023; San Diego, California.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.