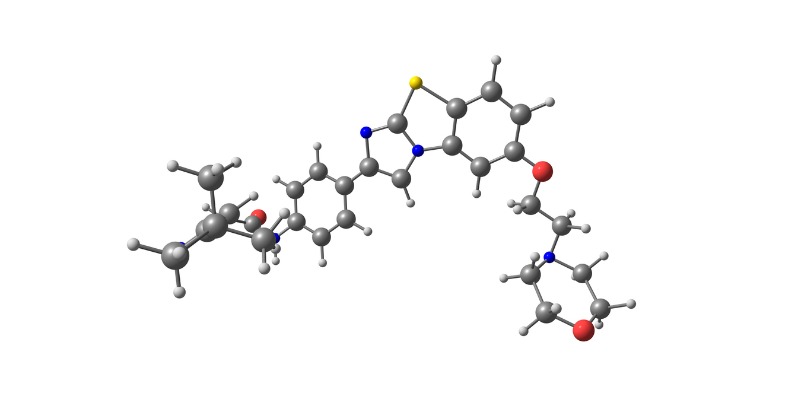
A review article published in the Journal of Hematology & Oncology by Jorge Cortes, MD, of the Georgia Cancer Center at Augusta University, outlines the efficacy, dosing, and safety of quizartinib for patients with FLT3-ITD–positive acute myeloid leukemia (AML). The novel, second-generation, highly potent, and selective type II FLT3 inhibitor is explored both as monotherapy and in combination with chemotherapy.
FLT3-ITD mutations, which occur in 25% of newly diagnosed AML cases, are associated with unfavorable outcomes, shorter survival, and increased risk of relapse by driving disease progression, Dr. Cortes explained. Quizartinib is approved in Japan as monotherapy and in the United States, Japan, Europe, and the United Kingdom as maintenance monotherapy and in combination with chemotherapy during induction and consolidation. However, it is not approved after allogeneic hematopoietic stem cell transplantation (HSCT) in the United States. Two phase III clinical trials, QuANTUM-R and QuANTUM-First, led to the drug’s approval.
QuANTUM-R Study
This phase III study evaluated quizartinib monotherapy versus salvage chemotherapy in 367 patients with FLT3-ITD–positive, relapsed or refractory AML who received prior anthracycline-containing induction chemotherapy. Salvage chemotherapy consisted of the following three physicians’ choice regimens: (1) low-dose cytarabine; (2) mitoxantrone, etoposide, and cytarabine (MEC); (3) fludarabine, cytarabine, and granulocyte colony-stimulating factor with idarubicin (FLAG-IDA).
Patients received quizartinib at a starting dose of 30 mg/day, then at 60 mg/day on day 16 if the corrected QT interval (QTc) remained at 450 ms or less during the previous 15 days. The median follow-up was 23.5 months.
Patients who received quizartinib had a statistically significant improvement in overall survival compared with patients who received chemotherapy (6.2 months vs 4.7 months, respectively; hazard ratio [HR], 0.76; 95%; CI, 0.58-0.98; P=.02). Quizartinib also achieved a nonstatistically significant improvement in median event-free survival (EFS) compared with chemotherapy (1.4 months vs 0.9 months, respectively; HR=0.90; 95% CI, 0.70-1.16; P=0.11).
QuANTUM-First Study
This phase III study evaluated quizartinib plus chemotherapy in induction and consolidation versus placebo, followed by up to three years of quizartinib or placebo single-agent continuation.
Patients received quizartinib (n=268) or placebo (n=271) at a starting dose of 40 mg/day on day 8 of the start of chemotherapy. Treatment continued until day 21. Those who did not achieve complete remission (CR) or complete remission with incomplete neutrophil or platelet recovery (CRi) could receive a second cycle of induction (7 + 3 or 5 + 2 regimens plus quizartinib or placebo). Those who achieved CR or CRi could receive consolidation with high-dose cytarabine plus quizartinib (40 mg/day) or placebo for 14 days of each cycle, beginning on day 6. After consolidation with cytarabine or allogeneic HSCT, placebo or quizartinib was allowed at a starting dose of 30 mg/day, then at an escalated dose of 60 mg/day after 15 days if the QTc remained up to 450 ms. The median follow-up was 39.2 months.
Adding quizartinib to chemotherapy demonstrated a statistically significant improvement in OS compared with standard induction and consolidation chemotherapy (HR, 0.776; 95% CI, 0.615-0.979; P=.0324). The median OS was 31.9 months for quizartinib versus 15.1 months for placebo. Quizartinib also showed a nonstatistically significant but favorable trend in EFS compared with placebo. Thirty-three patients achieved CR in the quizartinib arm between day 42 and the end of induction, compared with 18 patients in the placebo arm.
Safety
A black box warning for quizartinib includes QTc prolongation, torsades de pointes, and cardiac arrest, Dr. Cortes noted. Of the 265 patients treated with quizartinib in the QuANTUM-First study, 2.3% had an increase from baseline QTc according to the Fridericia formula (QTcF) greater than 500 ms, and 10.2% had a QTcF increase greater than 60 ms. Two (0.8%) patients experienced cardiac arrest, and no patient experienced torsades de pointes.
Of 1,081 patients from various clinical trials, 0.6% reported cardiac arrest, 0.2% reported torsades de pointes, and 0.1% reported ventricular fibrillation.
Dr. Cortes also outlined measures to minimize QTc prolongation risk, which include QTcF-based dose initiation and modification criteria, regular electrocardiographic monitoring, monitoring for and correcting risk factors such as serum electrolyte abnormalities, reducing or avoiding concomitant QT-prolonging medications according to label instructions, and reducing the quizartinib dose when administering concomitant strong inhibitors.
Other treatment-emergent adverse events with quizartinib observed in the QuANTUM-First study include febrile neutropenia, pyrexia, diarrhea, hypokalemia, nausea, headache, rash, vomiting, stomatitis, constipation, and neutropenia.
Ongoing Trials
Quizartinib is currently being evaluated in combination with other antineoplastic agents in clinical trials, in patients with FLT3-ITD–negative AML in both the first-line and relapsed or refractory settings, and in patients fit or unfit for intensive chemotherapy.
“Results of these ongoing studies may open new avenues for quizartinib approvals in FLT3-ITD–negative AML, as well as for patients unfit for intensive chemotherapy….It would be beneficial to further optimize the clinical value of quizartinib and find additional clinical settings for quizartinib use both in the frontline and salvage settings,” Dr. Cortes wrote.
Reference
Cortes J. Quizartinib: a potent and selective FLT3 inhibitor for the treatment of patients with FLT3-ITD–positive AML. J Hematol Oncol 2024;17(1):111. https://doi.org/10.1186/s13045-024-01617-7



 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.