Patients with myelofibrosis (MF) with high molecular and cytogenetic risk do not benefit from higher intensity conditioning before hematopoietic stem cell transplantation (HSCT), according to a retrospective analysis.
Both reduced intensity (RIC) and myeloablative (MAC) conditioning transplantation had comparable outcomes in patients with MF classified as high-molecular or cytogenetic risk, the investigators, led by Nico Gagelmann, MD, of the University Medical Center Hamburg-Eppendorf in Germany, said.
Dr. Gagelmann and colleagues conducted the study due to “limited information when comparing intensities according to different clinical but even more molecular and cytogenetic risk categories” and to be able to “recommend specific conditioning intensities” in patients with MF undergoing allogeneic HSCT.
The retrospective analysis included 645 genetically annotated patients (with at least driver mutation status available), of whom 414 received RIC and 231 received MAC. Patient data were collected from the following institutions:
- University Medical Center Hamburg-Eppendorf (Hamburg, Germany)
- West German Cancer Center (Essen, Germany)
- Hôpital Saint-Louis (Paris, France)
- Fred Hutchinson Cancer Research Center (Seattle, Washington)
- Hannover Medical School (Hannover, Germany)
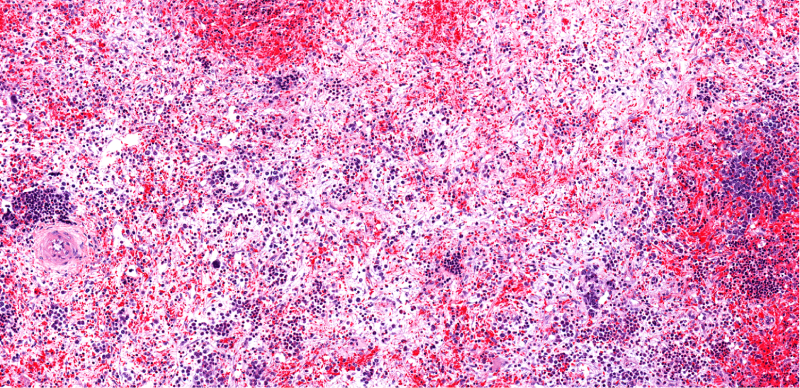
Patient bone marrow or peripheral blood samples were analyzed for the following MF-associated genes: JAK2, CALR, MPL, ASXL1, IDH1/2, CBL, DNMT3A, TET2, SF3B1, SRSF2, U2AF1, EZH2, TP53, NRAS, KRAS, RUNX1, and FLT3. Patients were considered high risk if they were positive for IDH1/2, SRSF2, AXSL1, or EZH2.
The study’s primary endpoint was overall survival (OS), and the secondary endpoints were non-relapse mortality, progression-free survival (PFS), and cumulative incidence of relapse.
The median time in months between diagnosis of MF and transplantation was 2.2 years (range, 0.01-47.3 years) in the RIC group and 1.4 years (range, 0.02-26.1 years) in the MAC group (P=.08). The median follow-up time was six years for RIC and nine years for MAC (see TABLE 1 for primary and secondary outcomes).
| TABLE 1. Outcomes in Patients in RIC and MAC Transplantation | |||
| RIC | MAC | P value | |
| Six-year OS rate | 63% (95% CI, 58-68) | 59% (95% CI, 52-66) | .34 |
| PFS | 52% (95% CI, 47-57) | 52% (95% CI, 45-59) | .64 |
The two-year cumulative incidence of non-relapse mortality was 26% (95% CI, 21-31) for RIC and 29% (95% CI, 23-34) for MAC (P=.51). In terms of progression/relapse, the two-year cumulative incidence was 10% (95% CI, 5-19) for RIC and 9% (95% CI, 4-14) for MAC (P=.46).
In addition, patients with reduced performance status, matched unrelated donors, and ASXL1 mutations appeared to benefit from RIC (see TABLE 2).
| TABLE 2. Patients Who Appeared to Benefit From RIC | ||
| Patient Subgroup | RR* | 95% CI |
| Younger patients | 0.68 | 0.48-0.97 |
| Matched unrelated donor transplants | 0.66 | 0.49-0.89 |
| Dynamic International Prognostic Scoring System intermediate-2 risk at time of transplant | 0.72 | 0.54-0.96 |
| Karnofsky performance status <90% | 0.74 | 0.55-1.00 |
| ASXL1 mutations | 0.80 | 0.58-1.09 |
| *RR, reduced risk of death in terms of OS. | ||
Limitations of the study include biases inherent to retrospective studies, which include different center practices and environments; a lack of transparency for physician choice of regimen intensity; and incomplete data on the patient level, the authors said.
“RIC and MAC showed, in general, comparable outcome in MF with available molecular-genetic information,” the authors concluded.
Reference
Gagelmann N, Salit RB, Schroeder T, et al. High molecular and cytogenetic risk in myelofibrosis does not benefit from higher intensity conditioning before hematopoietic cell transplantation: an international collaborative analysis. Hemasphere. 2022;6(10). doi:10.1097/HS9.0000000000000784





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.