SOHO 2024: Focus on Leukemia
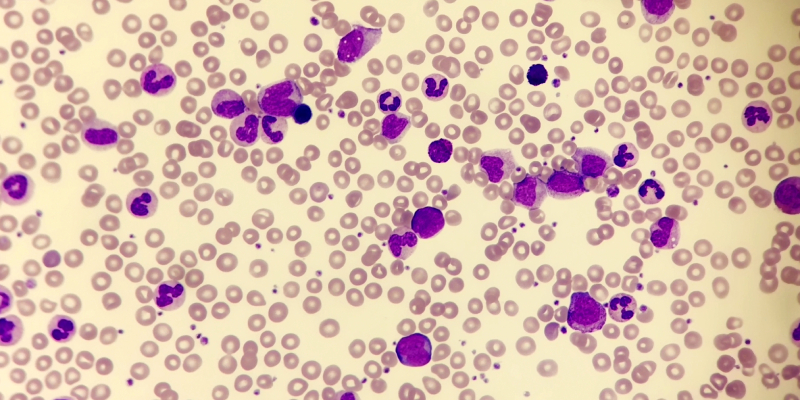
Adverse events were common in patients with CML receiving first- or second-generation tyrosine kinase inhibitors.
Venetoclax plus ibrutinib was associated with lower rates of mortality and serious adverse events than the control regimens.
MDS-related gene mutations and number of mutations did not correlate with worse outcomes.
Advertisement
The one-year overall survival rate of 90%, and the MRD negativity rate was 94%.
Ponatinib demonstrated long-term efficacy and manageable safety in patients with highly resistant, chronic phase CML.
Achieving deep molecular response has allowed for treatment discontinuation, making TFR a main goal of therapy.
Advertisement
Olverembatinib was well tolerated and showed strong antileukemic activity in patients with chronic phase CML.
Asciminib continues to demonstrate favorable safety and tolerability compared to TKIs in patients with chronic phase CML.
Age ≥65 years, arrhythmia, and cardiogenic shock were associated with a significantly higher rate of acute heart failure.
Liso-cel demonstrated clinical benefit and manageable safety, with low incidences of grade ≥3 CRS.
Length of venetoclax dosing and prior chemotherapy exposure were associated with prolonged hematological recovery.
The phase Ib/II FELIX trial found that obe-cel is effective for the treatment of relapsed or refractory adult B-cell ALL.
Fixed-duration ibrutinib plus venetoclax provides durable PFS in patients with CLL.
Ibrutinib provides significantly longer PFS and OS benefits in CLL when compared to chlorambucil.
Oral targeted inhibitors are a viable treatment for patients with CLL with severe renal dysfunction.
Switching rates within 60 days were lower for patients treated with zanubrutinib compared with acalabrutinib and ibrutinib.
Quizartinib significantly improves long-term survival in FLT3-ITD+ AML by achieving deep and sustained reductions in MRD.
Combining HMAs with venetoclax significantly improves remission rates and survival but requires more healthcare resources.
SLC40A1 mRNA levels were significantly higher in AML patients compared with controls and were associated with poorer OS.
Achieving complete hematologic recovery before subsequent treatment cycles is associated with improved survival outcomes.
















 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.