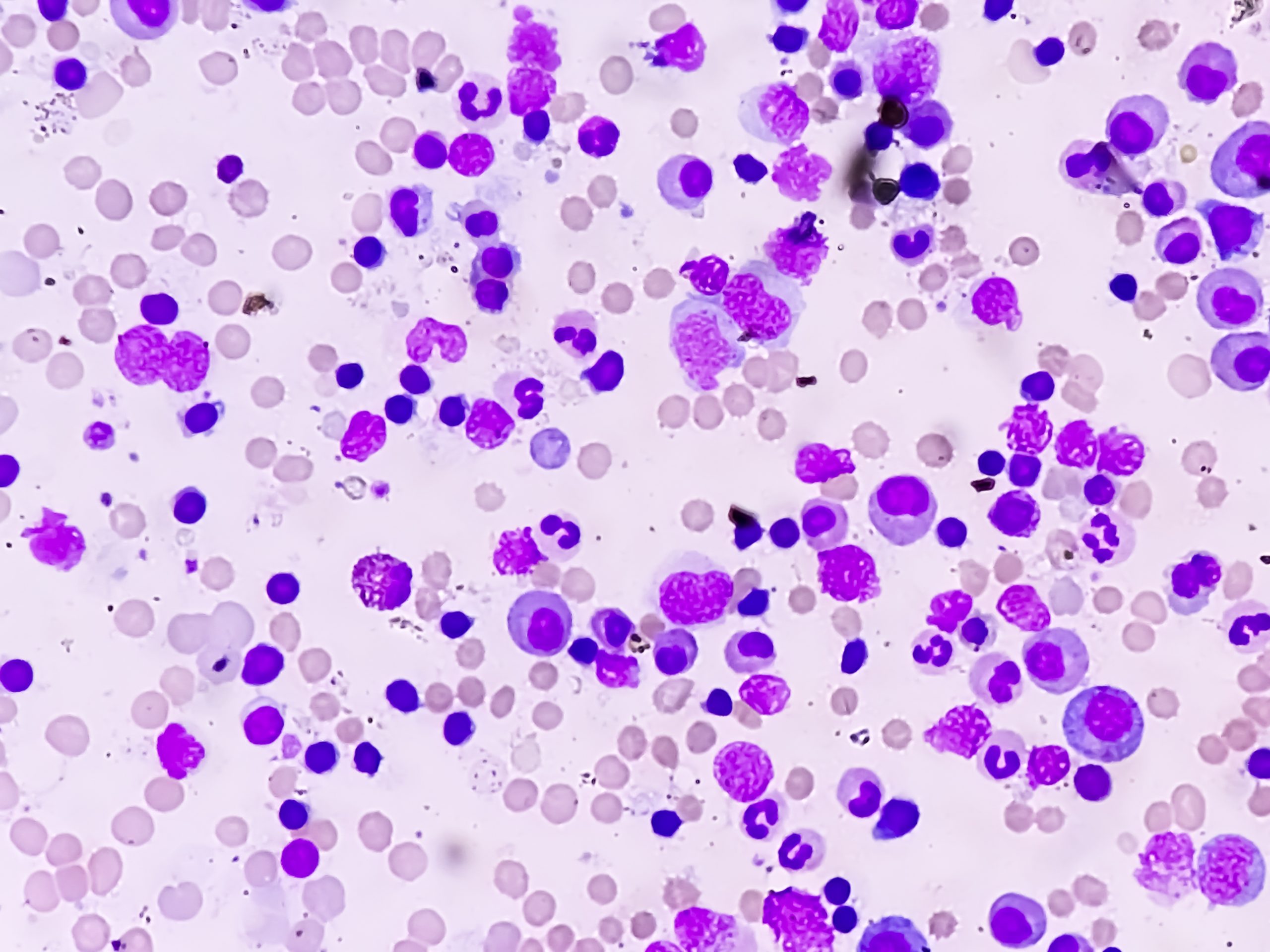
Azacitidine may be a treatment option for patients with systemic autoimmune and inflammatory disorders (SAID) associated with myelodysplastic syndromes (MDS) and chronic myelomonocytic leukemia (CMML), according to a phase II, prospective trial of azacitidine in steroid-dependent or -refractory SAID.
“[Azacitidine] may represent an interesting treatment for MDS/CMML patients with associated SAID, acting on both hematological disease and systemic inflammation,” the investigators, led by Arsene Mekinian, MD, of the Hospital Saint-Antoine Ap-Hp in Paris, France, wrote.
The open-label, single-arm, multicenter trial enrolled 29 patients with SAID manifestations of MDS/CMML who were steroid-dependent or -refractory. Twelve patients (41%) were retrospectively found positive for UBA1 mutation (VEXAS syndrome).
Patients received azacitidine 75 mg/m2 daily for seven days every four weeks for at least six cycles (or until overt disease progression or major side effects). At azacitidine onset, prednisone was administered at 1 mg/kg for one month, followed by a gradual tapering over six months at the physician’s discretion. After six cycles of azacitidine, prednisone was discontinued in the case of SAID complete response (CR).
Seven patients received less than six cycles of azacitidine due to death (n=2), toxicity (n=3), MDS progression (n=1), or the patient’s decision (n=1). After six cycles, 19 patients (66%) had a response in terms of SAID criteria, including eight CRs and 11 partial responses. Nine of 12 (75%) UBA1-mutated patients responded, as did 10 of 17 (59%) non-VEXAS patients. Azacitidine also yielded a hematological response in 59% of the patients, and 88% of hematological responders had a concomitant SAID criteria response.
The investigators also observed a sustained steroid-sparing effect of azacitidine, with a reduction to a median dose below 10 mg/day of prednisone equivalent after six cycles.
Dr. Mekinian and colleagues wrote that azacitidine could be used to manage UBA1 mutations in concomitant MDS.
“[Azacitidine] allowed rapid response with a decrease of inflammatory-related symptoms and daily prednisone equivalent dose in 75% of UBA1-mutated patients,” the authors wrote. “Therefore, [azacitidine] could be a treatment of choice for VEXAS management, especially in the subset of patients with concomitant MDS.”
Reference
Mekinian A, Zhao LP, Chevret S, et al. A phase II prospective trial of azacitidine in steroid-dependent or refractory systemic autoimmune/inflammatory disorders and VEXAS syndrome associated with MDS and CMML. Leukemia. 2022;36(11):2739-2742.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.