Further development of BI 836858 was discontinued after it failed to elicit a response in transfusion-dependent, low- or intermediate-1-risk myelodysplastic syndromes (MDS), according to a phase I/II trial.
“No conclusions on the efficacy of BI 835858 in patients with MDS could be drawn due to premature termination of the trial,” the investigators, led by Rami Komrokji, MD, of the Moffitt Cancer Center, wrote.
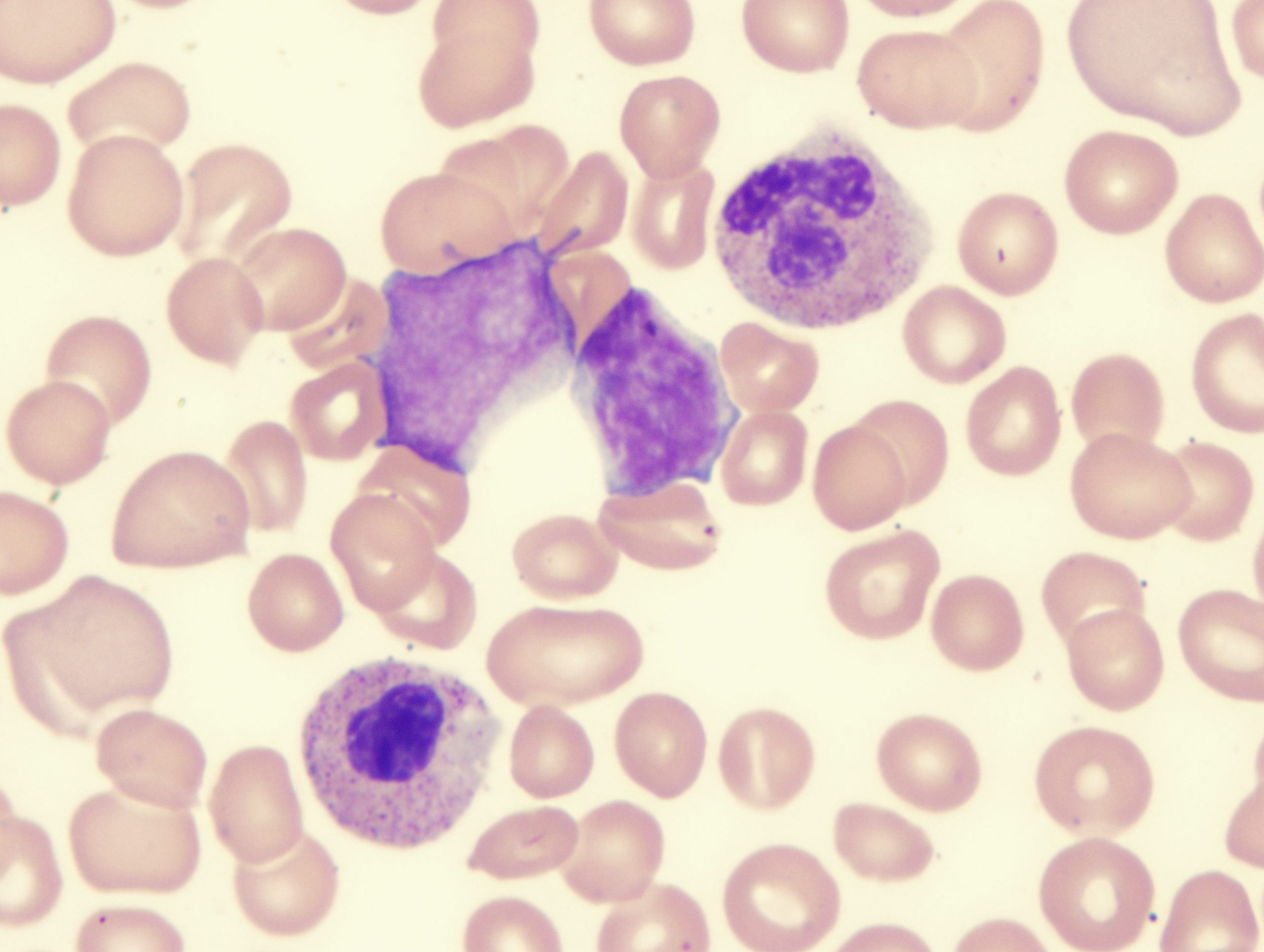
The open-label, dose-escalation study treated 27 patients with BI 836858, a fully humanized, immunoglobulin G1, unconjugated anti-CD33 monoclonal antibody. The median duration of treatment was 114 days (range, 1-811 days), and a median of five cycles were initiated (range, 1-29 cycles).
In phase I of the trial, BI 836858 was given as a rate-controlled intravenous infusion on days one and 15 of a 28-day cycle without premedication, with a starting dose of 20 mg and a max dose of 320 mg during the dose-escalation phase. Patients would be eligible to receive up to eight repeated administrations of the treatment, with an option to go beyond four cycles if they showed clinical benefit and had acceptable tolerability.
In phase II of the trial, patients would have been randomized to receive best supportive care alone or with BI 836858. However, phase II was not conducted, as the sponsor terminated the study based on a lack of single-agent efficacy (hematologic response) in the dose-escalation phase.
The trial included a pharmacodynamic analysis of the impact of BI 836858 on CD33 expression on myeloid-derived suppressor cells (MDSC). While the absolute number of CD33-postive MDSC decreased with treatment in some patients, CD33-negative leukocytes increased at the same time, indicating that BI 836858 either masked or internalized CD33 molecules on MDSC but did not reduce the number of MDSC.
Dr. Komrokji and colleagues reported that phase I of the trial demonstrated the feasibility and tolerability of MDSC-targeted approaches using CD33 as applied in transfusion-dependent lower-risk MDS. The maximum tolerated dose of BI 836858 was not reached at doses up to 320 mg in patients with low- or intermediate-1-risk MDS. Infusion-related reactions were the most commonly observed toxicity, which were grade ≥2 in 41% of patients. The overall adverse event profile was consistent with that expected for patients with MDS.
“It is unknown whether the lack of efficacy reflects a feature of the antibody itself, or whether targeting MDSC is insufficient to elicit an antitumor response,” the authors wrote. They speculated that alternative forms other than a “naked” anti-CD33 antibody (eg, antibody-drug conjugates or bispecific T-cell engaging antibodies) might be required to induce clinical efficacy.
BI 836858 was also assessed in a phase I dose-escalation study in patients with relapsed or refractory acute myeloid leukemia, but that study was also terminated prematurely.
Reference
Komrokji RS, Carraway HE, Germing U, et al. A phase I/II multicenter, open-label, dose escalation and randomized trial of BI 836858 in patients with low- or intermediate-1-risk myelodysplastic syndrome. Haematologica. 2022;107(11):2742-2747.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.