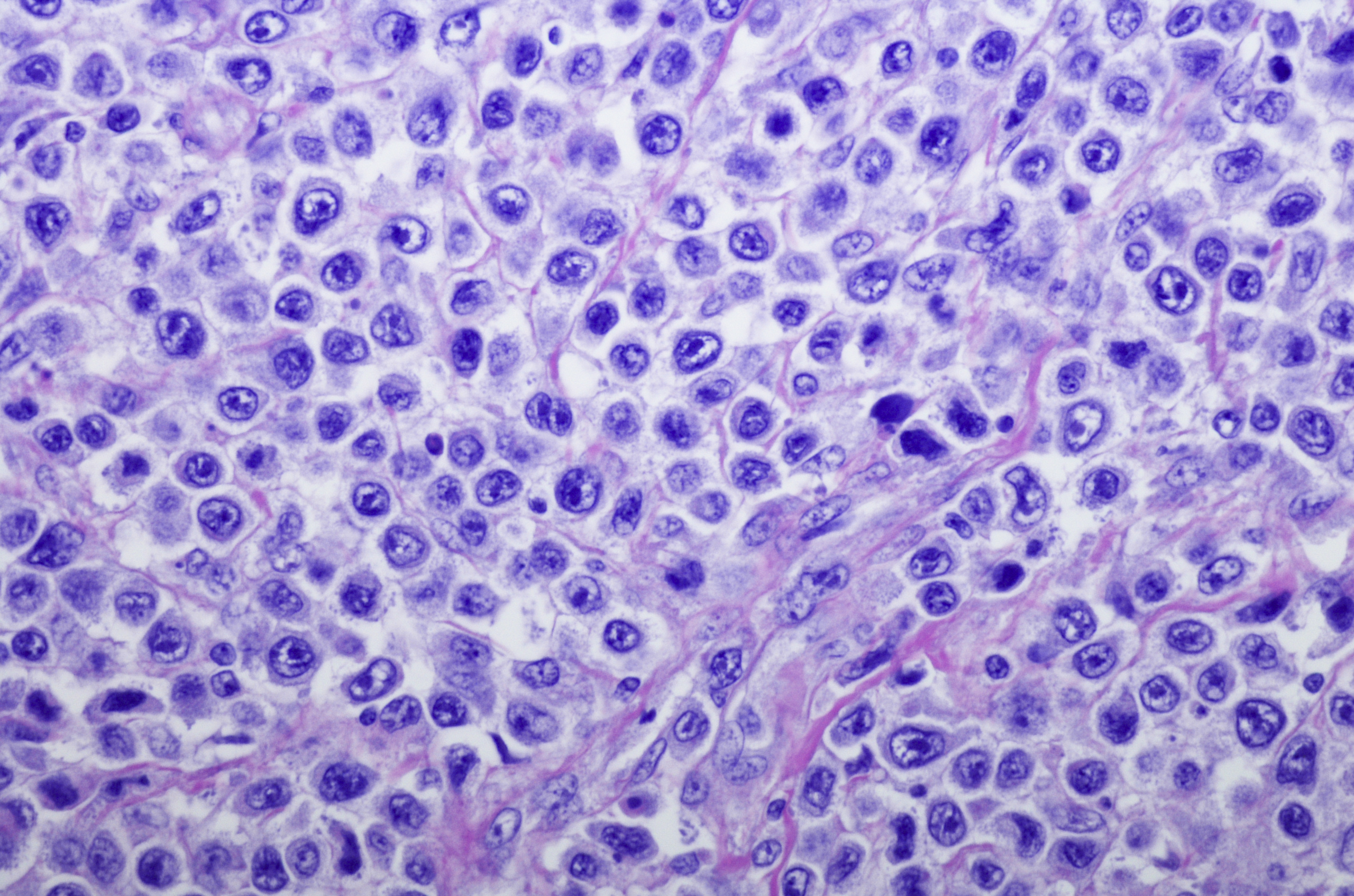
The addition of brentuximab vedotin (BV) to lenalidomide plus rituximab (R2) resulted in a statistically significant overall survival (OS) advantage over R2 alone in patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL).1
The median OS shown was 13.8 months (95% CI, 10.3-18.8) in patients treated with BV+R2 versus 8.5 months (95% CI, 5.4-11.7) in those treated with R2 alone, resulting in a 37% reduction in the risk of death (hazard ratio [HR], 0.629; 95% CI, 0.445-0.891; P=.0085), according to published results from the phase III ECHELON-3 study (NCT04404283). The OS benefit was consistent across the high-risk subgroups assessed in the study.
“The overall survival benefit of BV+R2 is clearly clinically meaningful and somewhat surprising given the modest PFS [progression-free survival] benefit. This is particularly true in this older patient population,” Craig A. Portell, MD, a study co-investigator and clinical faculty member, Division of Hematology/Oncology at the University of Virginia told Blood Cancers Today.
In terms of PFS, BV+R2 showed a median of 4.2 months (95% CI, 2.9-7.1) compared with a median of 2.6 months (95% CI, 1.4-3.1) with R2, achieving a 47% reduction in the risk of disease progression or death (HR, 0.527; 95% CI, 0.380-0.729; P<.0001).
The objective response rate observed with BV+R2 was 64.3% (95% CI, 54.7-73.1) versus 41.5% (95% CI, 32.5-51.0) in the R2-only arm (P=.0006). Complete responses were achieved in 40.2% of the BV+R2 arm compared with 18.6% of the R2 arm. The median duration of response was 8.3 months (95% CI, 4.2-15.3) with BV+R2 versus 3 months (95% CI, 2.8-5.4) with R2 alone.
Grade ≥3 treatment-emergent adverse events (TEAEs) were observed in 88% of patients in the BV+R2 arm compared with 77% of patients in the R2-alone arm, and serious TEAEs occurred in 60% versus 50%, respectively. Grade 5 TEAES occurred in 2% of the BV+R2 arm versus 8% of the R2 arm.
Portell stated that “while cytopenias were common, neutropenic fever was not, and there were no new safety signals that were seen.” In the BV+R2 arm versus the R2-only arm, investigators reported the most common TEAEs as neutropenia in 46% versus 32%, anemia in 29% versus 27%, and diarrhea in 31% versus 23%, respectively. Thirty-one percent of the BV+R2 arm had peripheral neuropathy compared with 24% of the R2 arm.
Efficacy and safety data from ECHECLON-3 come from a cohort of 230 patents with relapsed or refractory DLBCL, 112 of whom received BV+R2 and 118 of whom received R2 alone. All patients enrolled received at least one dose of study treatment, and the median duration of treatment was 3.6 months in the BV+R2 arm and 2.0 months in the R2-only arm. All patients had a median of three (range, 2–8) prior lines of therapy including prior chimeric antigen receptor (CAR) T-cell therapy.
Based on the findings at a median follow-up of 16.4 months (range, 0.1-31.5 months), investigators have deemed BV+R2 a novel therapeutic option for heavily pretreated, relapsed or refractory DLBCL. According to ECHELON-3 investigators, this is important, considering that patients with relapsed or refractory DLBCL who experience relapse after transplant or who are ineligible for transplant or CAR T-cell therapy have a poor prognosis.2
“I think we need to understand why BV added such a benefit in OS. Even with the target of BV, CD30 was not expressed. Hopefully, some correlative work with samples from the study will help with this,” said Portell.
References
- Bartlett N, Hahn U, Kim W, et al. Brentuximab vedotin combination for relapsed diffuse large B-cell lymphoma. J Clin Oncol. Published January 7, 2025. doi:1200/JCO-24-02242
- Bartlett N, Yasenchak C, Ashraf K, et al. Brentuximab vedotin in combination with lenalidomide and rituximab in patients with relapsed/refractory diffuse large B-cell lymphoma: safety and efficacy results from the safety run-in period of the phase 3 ECHELON-3 study. J Clin Oncol. 2022;40(16):suppl 7559. doi:1200/JCO.2022.40.16_suppl.755




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.