A retrospective study on the clinical outcome of myelodysplastic syndromes (MDS) progressing after treatment with hypomethylating agents (HMAs) showed that the response rate and survival outcome are still modest and highlighted the need for effective therapies to improve outcomes for these high-risk patients.
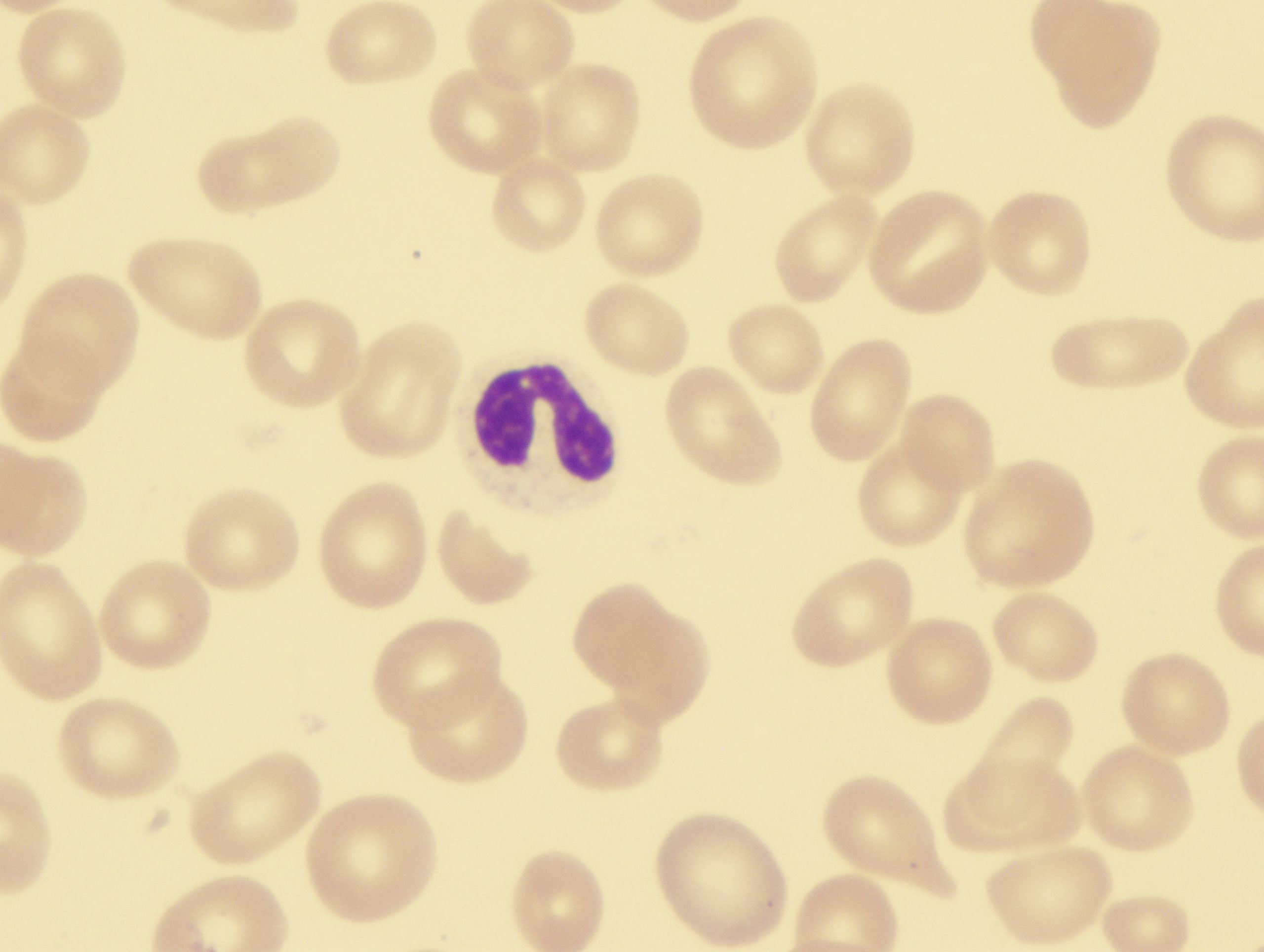
Two HMAs, azacitidine and decitabine, are currently approved by the US Food & Drug Administration and are the standard treatment of patients with higher risk MDS. However, overall response rates are modest, and a significant proportion of patients progress after HMA therapy. The majority of these patients carry adverse risk chromosomal/molecular features, are older, or are otherwise ineligible for intensive therapies and therefore have poorer prognoses.
Recently, azacitidine plus venetoclax-based therapy has been a paradigm shift in the management of patients with acute myeloid leukemia (AML) who are ineligible for intensive therapies. However, according to the retrospective study, the survival benefits of the combination remain modest.
The study included 71 MDS patients progressing on HMA therapy and treated at the Mayo Clinic. Patient clinical data included baseline characteristics and mutation analysis performed on bone marrow specimens using a 42-gene targeted next-generation sequencing panel. Patients’ treatment after HMA progression and clinical outcomes were extracted from their electronic medical records.
The median age was 67 years (range, 36-91 years), and 24% of patients (n=17) were diagnosed with therapy-related MDS (t-MDS) and 48% (n=34/71) with complex cytogenic abnormalities.
Median overall survival (OS) after progressing on HMA across the entire cohort was 7.4 months. After excluding five patients who did not receive further therapy after HMA progression, the median OS was 9.3 months, and the median OS after HMA progression based on therapy was 10.87 months.
The results showed that a venetoclax-based regimen was associated with better OS after HMA progression, although this result did not retain significance in multivariate analysis. The authors speculated that the lack of significance was due to the heterogenous patient population with a higher proportion of patients harboring TP53 mutation having t-MDS, unlike the patients in the clinical trials.
Patients who achieved remission and underwent allogeneic hematopoietic stem cell transplantation had better OS, but the result did not retain significance for better OS in multivariate analysis.
The authors singled out the TP53 mutation as a predictor of a significantly inferior complete response rate (P=.04). “In our analysis in the era of novel therapies, TP53 mutation retained poor prognostic significance with a dismal median OS of 2.6 months after progressing on HMA,” they wrote.
Overall, for MDS patients progressing after HMA in the era of novel therapies, the response rate and survival outcome remain modest, and effective therapies are needed to improve outcomes for these high-risk patients, according to the authors.
Ghorab A, Al-Kali A, Elliot M, et al. Clinical outcome of myelodysplastic syndrome progressing on hypomethylating agents with evolving frontline therapies: continued challenges and unmet needs. Blood Cancer J. 2022;12(6):93. doi:10.1038/s41408-022-00691-9




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.