Take-aways:
- A proposed new model predicts DLBCL relapse and survival better than the traditional IPI method.
- The proposed model is based on MTV, a robust, prognostic PET/CT imaging biomarker for DLBCL outcomes.
- The model could be employed in clinical practice and clinical trials.
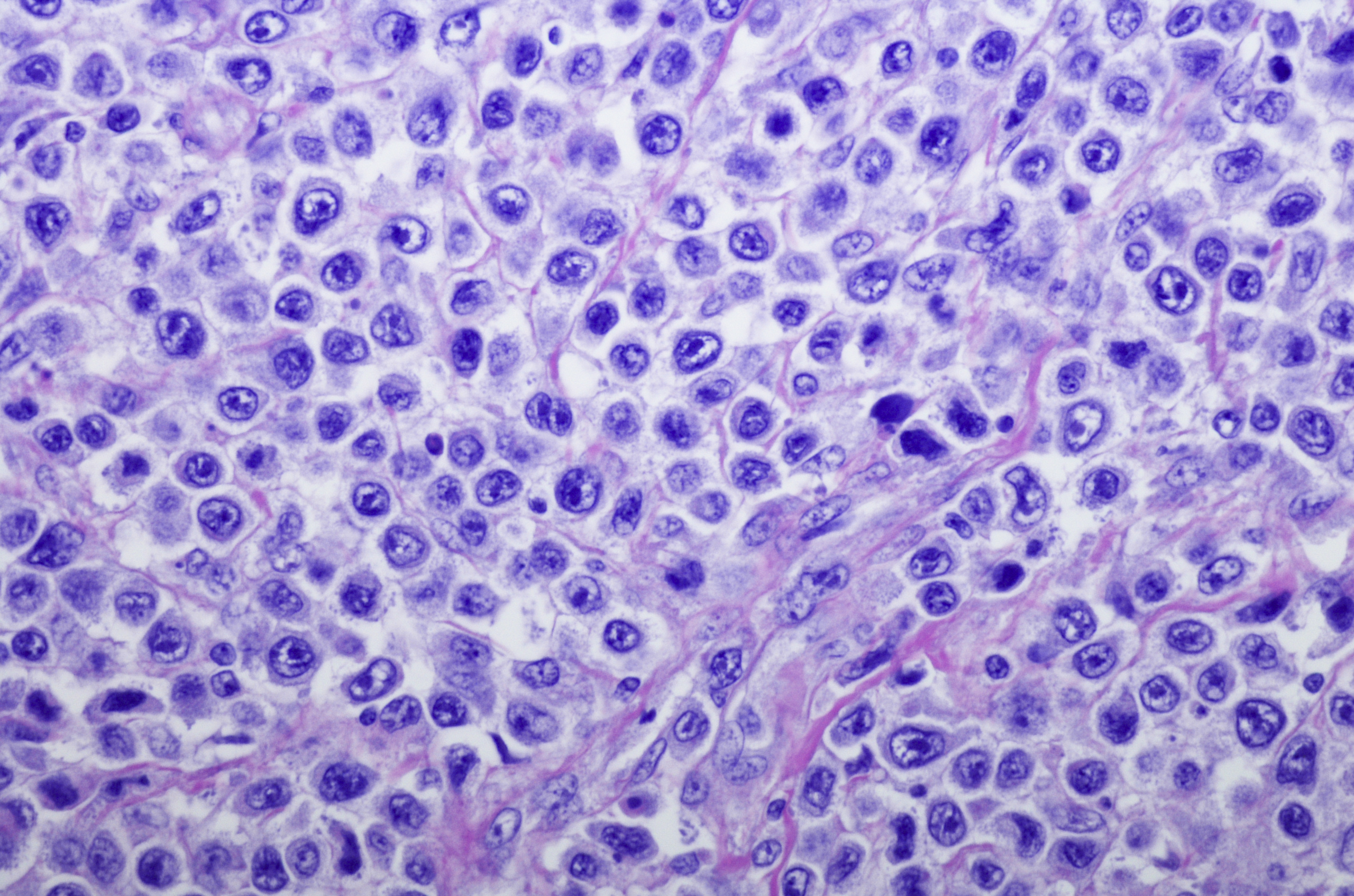
A new model that makes use of a promising imaging biomarker can predict diffuse large B-cell lymphoma (DLBCL) relapse and survival better than the traditional International Prognostic Index (IPI) model, enabling individualized estimates of patient outcomes, according to research published in the Journal of Clinical Oncology.
Called the International Metabolic Prognostic Index (IMPI), the proposed model centers on metabolic tumor volume (MTV), a measurement of total disease burden on 18-fluorine fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) imaging. MTV has been shown in prior research to be prognostic in several lymphoma subtypes, including DLBCL.
IMPI also encompasses two other factors: stage as a measure of disease dissemination and age reflecting the biologic reserve of the patient. MTV and patient age are combined as continuous variables with disease stage in a model that predicts relapse and survival better than the traditional IPI model, according to the researchers.
“This individualized level of prediction is more accurate than the traditional four IPI categories,” wrote N. George Mikhaeel, MD, of Guy’s Cancer Centre in London, and colleagues. “IMPI can be applied in clinical practice and clinical trials in a similar fashion to the standard IPI, [eg, to stratify patients for treatment comparisons or select patient groups with a defined prognosis to test new treatment approaches].”
Using MTV
Although MTV has performed robustly as a prognostic model for DLBCL and was reported to be independent of IPI for predicting patient outcomes, prior studies in the literature have not established how best to use this measurement. To determine the best expression of the relationship between baseline MTV and survival, the researchers studied 1,241 new patients with DLBCL from five published research studies with baseline FDG-PET/CT data. Three of the five studies were observational (GSTT15, NCRI, and SAKK) and two were randomized trials (HOVON-84 and PETAL), with no significant difference in progression or survival between treatment arms, which allowed the analyses to be combined.
The primary endpoint for modeling was three-year progression-free survival (PFS), defined as the time from baseline PET to progression, relapse, or death from any cause. Secondary endpoints were three-year overall survival (OS) and three-year time to progression (TTP).
Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone were given in 99% of the patients in the study. Three-year PFS was 74.5% (95% CI, 72.1-77.0), three-year OS was 81.8% (95% CI, 79.7-84.0), and three-year TTP was 79.7% (95% CI, 77.4-82.0) with a median follow-up of 55 months.
Modeling the Fit Between MTV and Survival
Dr. Mikhaeel and colleagues incorporated MTV into the IMPI model as a continuous rather than categorical variable based on the generalization that biomarkers predict outcomes better as continuous variables, and no simple linear relationship between MTV and survival exists. They examined the association of survival with MTV as a continuous variable using Cox regression models. Transformations of the MTV variable tested were cubic root transformation, natural log transformation, squaring, restricted cubic spline, and linear spline (LSP) models.
Three versions of the LSP model were tested: One with a single knot located at the median MTV (50th percentile), another with two knots at the 33rd and 66th percentiles, and a final version with three knots at the 10th, 50th, and 90th percentiles.
For each model, the fit between MTV and survival was evaluated with the Akaike information criterion (AIC) and the cross-validated c-index. To validate the robustness of the model, analyses were performed combining all five studies and repeated for the five separate study cohorts.
LSP Model
The results showed that the best relationship for MTV and survival, as measured by AIC, was an LSP model with a single knot located at the median MTV value of 307.9 cm3. The superiority of this model was validated with a leave-one-out cross-validation approach: Patients from four studies were used as the test set, and then validated in the fifth independent data set, according to a different study each time as the external independent validation set, for a total of five iterations.
Within each of the five cross-validation loops, the researchers identified overfitting in the regression coefficients of the best model by applying the trained linear predictor (slope) in the test data sets, and then used the slope value to correct the coefficients for overfitting.
MTV demonstrated a better fit to survival compared to IPI, as measured in terms of both higher c-index and lower AIC values, indicating that it is a better predictor of survival than the traditional IPI model. Across the three outcomes and the two criteria (AIC and c-index), no model performed uniformly best, but the combination of MTV with age and stage was always among the three best models and improved the prediction compared to the IPI model for both OS and TTP.
The model that performed best combined MTV with age as continuous variables and individual disease stage. It not only outperformed IPI, but also better defined a high-risk group of patients. Finally, a regression formula was used to estimate individual probabilities of patient survival.
The researchers noted that models incorporating performance status, serum lactate dehydrogenase, and extranodal sites, which are parameters of the traditional IPI model, did not add to the prediction of endpoints in the modeling results.
“This is the first study, to our knowledge, to incorporate MTV as a continuous variable and to show that LSP is the best function to express the relationship between MTV and survival rather than a linear relationship and provide individualized risk estimates,” the authors wrote.
Reference
Mikhaeel NG, Heymans MW, Eertink JJ, et al. Proposed new dynamic prognostic index for diffuse large B-cell lymphoma: International Metabolic Prognostic Index. J Clin Oncol. 2022. doi:10.1200/JCO2102063





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.