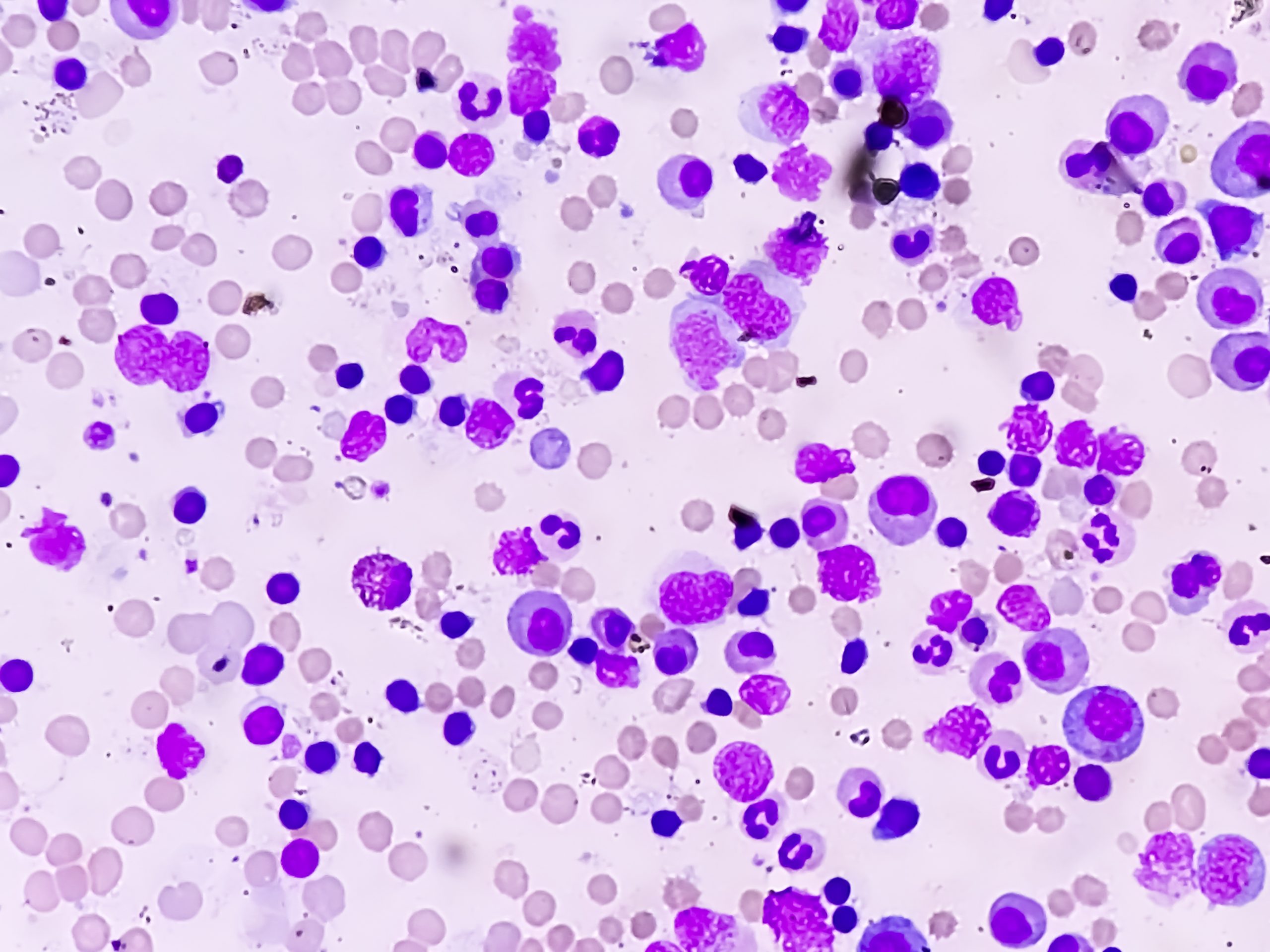
An analysis assessed clinicopathologic characteristics of patients with myelodysplastic syndromes (MDS) who experience hypomethylating agent failure (HMA-F) and observed high-risk features in this patient population, including higher bone marrow blasts, worsening thrombocytopenia, and more genomic aberrations.
Kelly Chien, MD, of the University of Texas MD Anderson Cancer Center, discussed her team’s research findings during the Society of Hematologic Oncology (SOHO) Annual Meeting.
Dr. Chien and colleagues retrospectively assessed 135 untreated patients with MDS who were diagnosed between 2017 and 2021 and later developed HMA-F. Median patient age at diagnosis was 70 years, and 39% of patients had therapy-related MDS. Most patients had higher-risk MDS per the Revised International Prognostic Scoring System (IPSS-R): 30% had high and 42% had very-high risk disease. Nearly half of patients (47%) had complex karyotype. Patients had a median of two mutations, the most common of which were TP53 (46%) and ASXLI (21%).
A majority of patients (67%) received HMA monotherapy, while 33% received an HMA in combination with other therapeutics; the median number of HMA cycles received was seven (range, 1-37 cycles). Patients were assessed at diagnosis and HMA-F.
At the time of HMA-F, patients had higher bone marrow blasts (P<.001), lower platelet counts (P<.001), and more cytogenetic abnormalities (P=.002) and mutations (P<.001) than at diagnosis.
Median time from diagnosis to HMA-F was 10.6 months, and median overall (OS) survival from HMA-F was 6.5 months. Survival was 17.8 months in lower-risk IPSS-R patients versus 3.8 months in higher-risk patients (P<.001). Median OS did not differ based on number of HMA cycles, response to HMA, or treatment regimen at HMA-F. In patients with higher-risk MDS, stem cell transplant (P<.001) was associated with improved median OS, while upfront HMA combination therapy (P=.008) was associated with inferior survival.
The authors noted that the findings indicate that patients with HMA-F MDS have high-risk features that are often therapy-related, and this patient population has a poor prognosis.
“Further understanding of the underlying biology of HMA-F MDS is warranted with an urgent need for therapeutic interventions after failure of HMA therapy,” the authors noted.
Reference
Chien K, Kim K, Li Z, et al. Disease characteristics and outcomes of hypomethylating agent failure in patients with myelodysplastic syndromes. Abstract #MDS-407. Presented at the 2022 Society of Hematologic Oncology (SOHO) Annual Meeting, September 28-October 1, 2022.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.