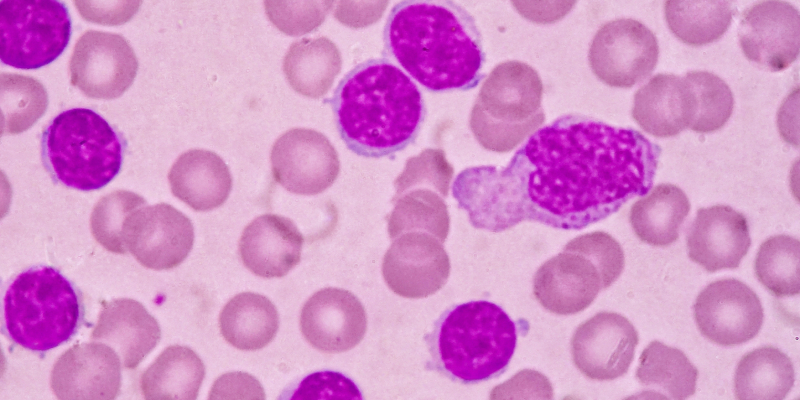
Pirtobrutinib achieved a 46% reduction in the risk of disease progression or death compared with idelalisib plus rituximab or bendamustine (IdealaR/BR) in heavily pretreated patients with relapsed or refractory chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL) who previously received a covalent Bruton tyrosine kinase inhibitor (BTKi).
Results come from the phase III BRUIN CLL-321 clinical trial, which is the first randomized phase III study to evaluate the efficacy and safety of pirtobrutinib in a cohort of patients previously treated with a covalent BTKi, according to lead investigator, Jeff P. Sharman, MD, director of research, the Willamette Valley Cancer Institute, and medical director of hematology research, The US Oncology Network.
“The median age of a patient in the United States treated for CLL is about 74 years old. Of course, there’s a broad diversity and there are patients who are both younger and older. But the younger a patient is and the more aggressive their disease is, the more likely they are going to have a relapse. We know that for many patients, they will cycle through more than one therapy. So, it’s not just going to be a BTK inhibitor alone, they may need a BTK then eventually need a BCL2 inhibitor,” explained Sharman.
The post-covalent BTKi or third-line setting for patients with CLL or SLL has an unmet need for new therapies, according to Sharman and colleagues. Pirtobrutinib is a noncovalent BTKi, which has been shown to inhibit both wild-type and C481-mutant BTK. Its potency has been shown to be equally low in each alteration, and it has demonstrated steady-state plasma exposure, which is associated with 96% BTK target inhibition and a 20-hour half-life.
The preclinical efficacy shown with pirtobrutinib was tested in 119 of 238 patients in BRUIN CLL-321. The remaining 119 patients were randomized to the IdealaR/BR arm. Progression-free survival (PFS) was assessed by independent review committee (IRC) after a median follow-up of 19.4 months in the pirtobrutinib arm and 17.7 months in the control arm. The median PFS was 14.0 months (95% CI, 11.0-16.6) with pirtobrutinib versus 8.7 months (95% CI, 8.1-10.4) with IdealaR/BR (hazard ratio [HR], 0.58; 95% CI, 0.38-0.89; P =.01).
The risk of an event was also decreased by 61% among patients treated with pirtobrutinib at a median follow-up of 19.4 months in the experimental arm and 18.7 months in the control arm (HR, 0.39; 95% CI, 0.28-0.53; stratified log-rank 2-sided P<.0001).
The median duration of follow-up for time to next treatment or death was 20.0 months in the pirtobrutinib arm and 20.2 months in the IdealaR/BR arm. The median time to next treatment was 24.0 months (95% CI, 17.8-29.7) with pirtobrutinib compared with only 10.9 months (95% CI, 8.7-12.5) with IdealaR/BR, resulting in a 63% reduction in risk of starting next treatment or death (HR, 0.37; 95% CI, 0.25-0.52; stratified log-rank 2-sided P<.0001).
At a median follow-up of 20.4 months in the pirtobrutinib arm and 19.2 months in the IdealaR/BR arm, the 18-month overall survival rate was 73.4% (95% CI, 63.9%-80.7%) and 70.8% (95% CI, 60.9%-78.7%), respectively (HR, 1.09; 95% CI, 0.68-1.75; stratified log-rank 2-sided P =.7202). Notably, 76% of patients receiving IdealaR/BR crossed over to the pirtobrutinib arm.
“There was benefit to the drug even beyond IwCLL criteria for progression, and I think the punch line there is that this is a molecule that is effective. It can control the disease for a length of time,” said Sharman about the efficacy findings.
Treatment-emergent adverse events (TEAEs) of any grade were observed in 93.1% of the pirtobrutinib arm versus 98.2% of the control arm. Grade 3 or higher TEAEs were seen in 57.7% of the pirtobrutinib arm versus 73.4% of the IdealaR/BR arm. Treatment-related AEs led to treatment discontinuation in 5.3% of the pirtobrutinib arm versus 21.1% of the control arm. Any-grade AEs of interest for pirtobrutinib included bleeding (21.6%), anemia (20.7%), neutropenia (26.7%), thrombocytopenia (9.5%), infection (63.8%), atrial fibrillation and atrial flutter (2.6%), and hypertension (6.9%).
“The basics of this study is to get approval for pirtobrutinib following a covalent BTK inhibitor. Theoretically, that means it could move up to second or third line,” explained Sharman. “Currently it’s approved as following prior covalent inhibitor and BCL2 inhibitor. This potentially allows patients to access the drug early. And of course, we’re awaiting regulatory decision-making on that,” he added.
References
Sharman JP, Munir T, Grosicki S, et al. BRUIN CLL-321: randomized phase III trial of pirtobrutinib versus idelalisib plus rituximab (IdelaR) or bendamustine plus rituximab (BR) in BTK inhibitor pretreated chronic lymphocytic leukemia/small lymphocytic lymphoma. Blood. 2024;144(suppl 1):886. doi:10.1182/blood-2024-198147




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.