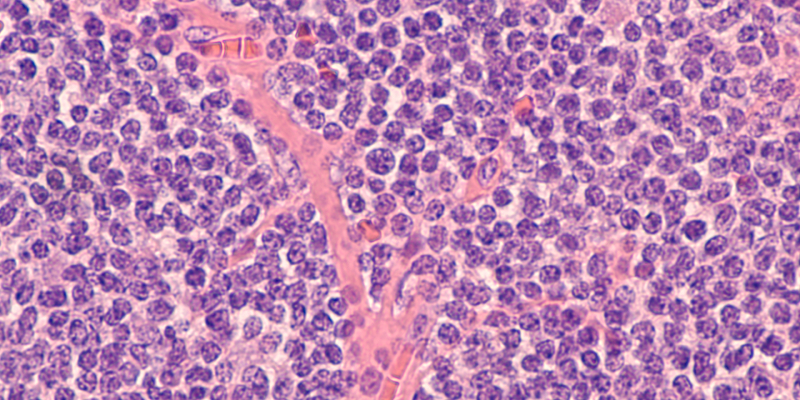
As per recent research, pirtobrutinib continues to demonstrate efficacy and safety in heavily pretreated patients with relapsed or refractory mantle cell lymphoma (MCL) who had prior therapy with a covalent Bruton tyrosine kinase inhibitor (cBTKi).
The study was led by Jonathon B. Cohen, MD, MS, of the Winship Cancer Institute at Emory University in Atlanta, Georgia, who reported updated results from the BRUIN trial.
BRUIN is a multicenter, phase I/II trial that administered pirtobrutinib monotherapy to 152 patients with MCL with a median of three prior lines of therapy, including an anti-CD20 antibody (96.7%), chemotherapy (90.1%), an immunomodulator (17.1%), stem cell transplantation (21.7%), a BCL2 inhibitor (15.8%), chimeric antigen receptor (CAR) T-cell therapy (8.6%), and a PI3K inhibitor (3.9%).
50% of patients had TP53 mutations, and 71% of patients had a Ki-67 index of ≥30%. The median age was 70 years, and 52% of patients had intermediate-risk sMIPI scores (Simplified Prognostic Index for Advanced-Stage Mantle Cell Lymphoma), whereas 28.3% had high-risk sMIPI scores.
Dose escalation ranged from 25–300 mg/day, with 141 patients (93%) receiving at least one dose of 200 mg/day, the dosage approved by the US Food and Drug Administration (FDA).
For patients pretreated with a cBTKi, the overall response rate (ORR) was 49.3%, including 15.8% complete response and 33.6% partial response. The 18- and 24-month duration of response (DOR) rates were 51.9% and 38.9%, respectively. Meanwhile, the ORR was 85.7% for cBTKi-naïve patients, and the 18- and 24-month DOR rates were both 90%.
High ORRs occurred in patients who had disease progression on a prior cBTKi, as well as in patients with high-risk disease features. Those features included elevated Ki-67 index (ORR 44.4%), TP53 mutations (ORR 43.3%), and blastoid and pleomorphic variants (ORRs 40% and 47.1%, respectively).
The most frequent treatment-emergent adverse events (AEs) were fatigue (31.9%), diarrhea (22.3%), and dyspnea (17.5%). The rate of grade ≥3 infections was 19.9%, most commonly neutropenia/neutrophil count decrease (13.3%). Eight patients (5%) had treatment-related AEs that led to dose reductions, and five patients (3%) had treatment-related AEs that led to pirtobrutinib discontinuation.
Reference
Cohen J, Shah N, Jurczak W, et al. Pirtobrutinib in relapsed/refractory (R/R) mantle cell lymphoma (MCL) patients with prior cBTKi: safety and efficacy including high-risk subgroup analyses from the phase 1/2 BRUIN study. Abstract #981. Presented at the 65th ASH Annual Meeting and Exposition; December 9–12, 2023; San Diego, California.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.