
Take-aways:
- Current prognostic scoring systems for MDS, such as the IPSS-R, may classify certain cases as lower-risk MDS, despite the presence of high-risk features.
- Lower-risk MDS with high-risk features may require a different treatment approach, making it critical to optimize prognostic tools that allow clinicians to balance the risk of therapy with the risk of the disease.
- Current prognostic scoring systems for MDS could be improved by incorporating relevant clinical features, molecular data, etiological information, and other factors.
Low-risk myelodysplastic syndromes (MDS) can have high-risk features, but current prognostic scoring systems for MDS may not capture key variables that impact risk and treatment outcomes in patients with lower-risk MDS, according to a recent perspective published in the Expert Review of Hematology.
Amy E. DeZern, MD, MHS, and William Brian Dalton, MD, PhD, of the Sidney Kimmel Comprehensive Cancer Center and The Johns Hopkins University School of Medicine, reviewed the literature on diagnostics, prognostics, therapeutics, and outcomes in patients with MDS because accurate prognostication is “especially important” in MDS, a heterogenous condition with varied survival.
MDS is “distinct from other cancers” as diseased cells in MDS “still serve a productive role for patients, however feebly,” which means MDS therapies must contend with potential “on-target effects of eliminating the mutant blood system,” Drs. DeZern and Dalton said in the review article.
“Thus, the limited but available treatments in MDS must be carefully timed along the disease trajectory so that their potential benefits to both quantity and quality of life outweigh their potential risks,” they wrote. “Given this, precise disease prognostication is imperative.”
Current MDS Prognostic Scoring Systems: Advantages and Limitations
It is critical to identify high-risk features in patients who have otherwise lower-risk MDS, as management of lower-risk disease is “generally conservative,” and “underestimating the risk of progression may miss the optimal time to initiative more aggressive treatments,” the review’s authors wrote.
Several MDS prognostic scoring systems are available, including the World Health Organization classification-based Prognostic Scoring System (WPSS), the MD Anderson Risk Model Score (MDAS), the MDS Lower-Risk Prognostic Scoring System (LR-PSS), and the revised International Prognostic Scoring System (IPSS-R).
The IPSS-R for MDS, which has been the “most widely adopted risk-stratification system” has advantages including updated cytogenetic risk groups, validation in multiple independent groups, validation in treated patients, and “evidence that it directly outperforms other scoring systems in some populations,” the review’s authors wrote.
However, the IPSS-R for MDS has “limitations in prognostic power,” particularly in patients with lower-risk disease, Drs. DeZern and Dalton wrote. For example, 7% of patients classified as lower risk by the IPSS-R were classified as high risk by the WPSS system, and 29% of patients classified as lower risk by IPSS-R were classified as high risk by the MDAS system.
Each system has its relative advantages and limitations, but the current systems “may fail to capture important prognostic information at the individual level due to the lack of incorporation of salient clinical features, molecular data, and dynamic changes in risk over time,” Drs. DeZern and Dalton wrote.
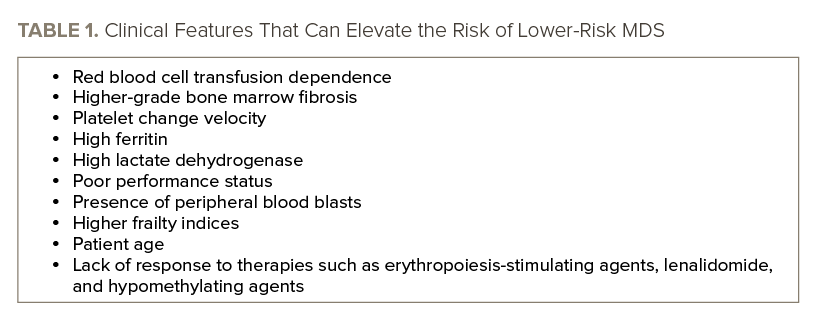
Specific Clinical Features Elevate MDS Risk
Certain clinical features may elevate the risk of lower-risk MDS, particularly red blood cell transfusion dependence, which independently predicts poor prognosis and adds prognostic value to the IPSS-R. Higher grade bone marrow fibrosis can also “signal poorer outcomes in lower-risk MDS,” according to the review. See TABLE 1 for a list of clinical features that can elevate the risk of lower-risk MDS.
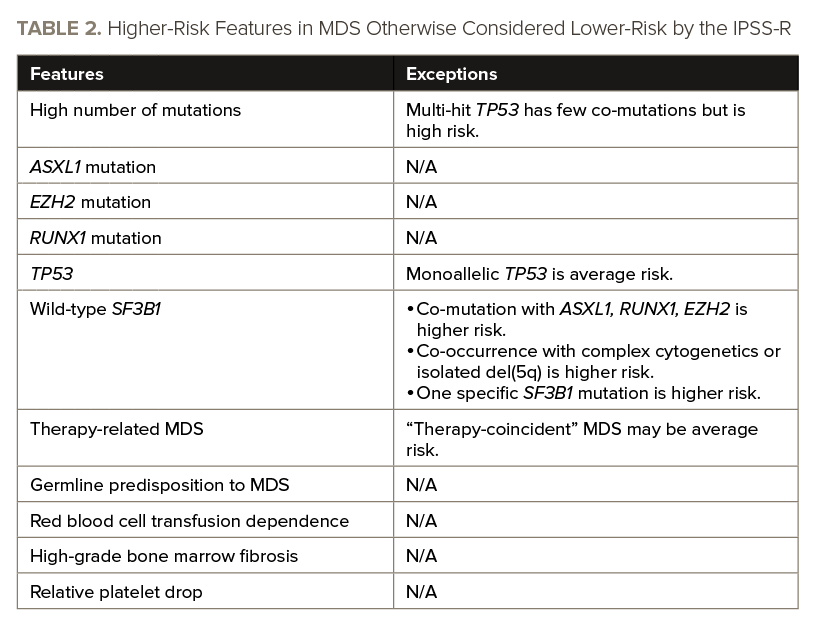
Mutation Quantity, Type, and Context Can Shape MDS Risk Level
Most patients with MDS have mutations and “clear examples of their independent prognostic utility have been well-documented,” Drs. DeZern and Dalton wrote. Despite this evidence, the “most notable deficiency” of all the validated scoring systems is the “lack of incorporation of gene mutations gleaned from next-generation sequencing,” they wrote.
The quantity and type of mutations can both play a role in shaping risk.
For example, the total number of driver mutations is negatively correlated with leukemia-free survival in patients with MDS, and the quantity of mutations has independent prognostic value for IPSS categories. Furthermore, an increasing number of mutations negatively correlates with leukemia-free survival and overall survival.
“Thus, IPSS-R lower-risk patients with elevated driver mutation number, especially those with three or more, are generally accepted as higher-risk and deserving of more proactive therapy,” Drs. DeZern and Dalton wrote.
Specific gene mutations are also associated with varying risk levels, with multiple studies showing mutations in certain genes can have prognostic value. For example, mutations in ASXL1, EZH2, RUNX1, and TP53 were “most consistently identified as predictive of negative outcomes,” Drs. DeZern and Dalton wrote.
Wild-type SF3B1 is associated with negative outcomes in patients with MDS, while mutations in SF3B1—which are present in more than 80% of cases of MDS with ring sideroblasts—are independent predictors of “more favorable outcomes,” according to the review’s authors.
However, there are “important exceptions that warrant consideration in risk assessment,” they wrote, as the impact of the mutation may be context dependent. For example, SF3B1 mutations are associated with poorer survival in patients with complex cytogenetics and in patients with isolated del(5q).
In the case of TP53 mutations, patient risk can vary with the allelic state of TP53. Patients with more than one TP53 mutation, chromosome 17 monosomy or 17p deletion, and high total TP53 variant allele frequency, are considered high-risk patients. However, patients who have one TP53 mutation, a lack of chromosome 17 abnormalities, lower variant allele frequency, and more co-mutations in other genes are considered average-risk patients.
“The clinical implications of these findings are clear: The allelic state of TP53 should be incorporated into the risk stratification” of patients with MDS, Drs. DeZern and Dalton wrote.
MDS Etiology Can Impact Risk
While the IPSS-R does not “incorporate the underlying etiology” of MDS, there is “evidence that the cause(s) of a patient’s MDS may be relevant to their prognosis independently of other established risk factors,” the review’s authors wrote.
For example, the IPSS-R for MDS has “less precision in prognosis” when applied to patients with therapy-related MDS, as those patients “generally have poorer outcomes” than patients with non-therapy-related MDS in the same IPSS-R risk group, according to Drs. DeZern and Dalton.
“Current evidence indicates that, in general, IPSS-R low-risk [therapy-related] MDS will likely be higher risk,” they wrote, noting further research is needed to determine the role of factors such as high-risk mutations, comorbidities, and sequalae of previous therapies in therapy-related MDS.
A germline predisposition to MDS, which can occur as part of a syndrome or an isolated myeloid disease, could also impact a patient’s prognosis. For example, in syndromic cases, which are “likely presenting earlier and with more IPSS-R low-risk disease due to increased surveillance” there may be a reason to believe they are higher-risk due to the “potential lead-time bias,” Drs. DeZern and Dalton wrote.
They suggested additional reasons why there may be a higher risk in patients who are otherwise low risk but have a germline predisposition to MDS. These reasons include “idiosyncratic pathologic and genetic features not captured by standard assays or scoring systems; tendency to develop additional, independent myeloid malignancies; syndromic comorbidities; increased disease-related toxicities from therapies; and the simple observation of poor MDS outcomes in relevant patient series.”
Therapeutic Considerations in Lower-Risk MDS with High-Risk Features
While standard treatments for lower-risk MDS are still currently used “regardless of higher-risk features,” Drs. DeZern and Dalton “emphasize the frequent need for reassessment if responses to treatment are not positive.”
Hypomethylating agents and lenalidomide are not approved for lower-risk MDS in many countries, but those therapies are “considerations in disease that has upstaged or has the adverse molecular features noted,” they wrote.
“For example, patients with multilineage dysplasia, pancytopenia, or greater than three mutations are often treated much earlier with [hypomethylating agents], regardless of IPSS-R lower scores,” Drs. DeZern and Dalton noted.
Transplantation may even be an option for certain patients with lower-risk MDS who have high-risk features.
“Historically, [bone marrow transplant] has been reserved for patients with higher-risk MDS, given its potential curative benefit is offset by the morbidity and mortality that can result from the procedure,” the review’s authors wrote. “Nonetheless, efforts have been made to weigh the toxicities of this intervention in [lower-risk] MDS and many [lower-risk] patients are offered [bone marrow transplant], especially those with higher-risk molecular features such as RUNX1, TP53, or ASXL1.”
The Future of MDS Prognostic Scoring Systems
Drs. DeZern and Dalton emphasized the need for new prognostic scoring systems that incorporate parameters on additional clinical features, molecular data, etiological information, and other variables discussed in the review. See TABLE 2 for an overview of features that can elevate the risk of lower-risk MDS.
They referenced two approaches that were published in The Journal of Clinical Oncology in 2021, one of which modeled clinical and genomic variables including mutations to generate a personalized prognostic assessment, and another of which used clinical and mutational data to develop a personalized prediction model. Both approaches “outperformed” the IPSS-R for MDS in independent datasets and “both groups intend to make their personalized prediction tools available online for application to individual MDS patients,” Drs. DeZern and Dalton wrote.
A large multi-institutional group has proposed a Molecular IPSS (IPSS-M) based on an analysis of clinical, cytogenetic, and mutational features from nearly 3,000 patients. This system changes stratification from the MDS IPSS-R classification in nearly half of patients, including 6% of patients who were classified as very low/low-risk by the IPSS-R for MDS and were reclassified as very high/high-risk by the IPSS-M.
“Implementation of these tools should launch a new era of molecular prognostication of low-risk MDS,” Drs. DeZern and Dalton wrote.
The authors also noted that there are “several areas where the precision of MDS prognosis can likely be further refined.” These areas include:
- Considering the prognostic value of individual variants of mutated genes.
- Investigating the impact of mutation variant allele frequency on prognosis.
- Understanding how less frequent mutations and cytogenetic abnormalities contribute to prognosis.
- Evaluating prognostic context dependence on various combinations of genetic and clinical features.
“Finally, there will likely be new disease parameters that bear on MDS prognosis in ways that we do not even incorporate clinically at present,” Drs. DeZern and Dalton wrote. “These include variables like DNA methylation, gene expression, RNA splicing, and measures of the ‘immunome,’ among others. With the tools available to us now, the field of MDS prognostication in the next 50 years promises to be even more exciting than the last.”
Experts Provide Opinion on Prognostic Scoring System Needs in Lower-Risk MDS
With the heterogeneity of lower-risk MDS and the need for accurate risk stratification to balance the risks and benefits of treatment, it is critical to develop and refine prognostic tools.
“Currently available prognostic scoring systems aid in risk stratification but do not capture all important variables, and they are also insufficient for prediction of response to therapy,” Drs. DeZern and Dalton wrote.
They believe the “goal is a proactive approach” in all lower-risk patients that will “extend quantity of life with quality through use of all available treatments,” as lower-risk MDS “requires an optimized understanding of a patient’s risk, as the risk of therapy must not exceed the risk of the disease in its current form.”
While treatment can vary—from observation and supportive treatments to active chemotherapy and allogeneic hematopoietic stem transplantation—based on the severity of the disease, these approaches may not be applicable to every case, Drs. DeZern and Dalton wrote.
It’s critical to understand the biology and natural history of the disease, as that information can help predict the likelihood of an adverse outcome and determine the appropriate intervention.
“In the future, incorporation of molecular profiling in both diagnosis, prognosis and formal classification/prognostication schemes will be paramount to help establish initiation of therapeutic interventions to alter the natural history of these syndromes,” the review’s authors wrote.
Integrating clinical data with diagnostic genome profiling can “then provide prognostic predictions that are tailored to individual patients and their dynamic course with a myeloid disorder,” they wrote.
“A key corollary to this personalized prognostic approach over the coming five years must be an active and growing portfolio of standard and investigational therapeutics to empower the clinician to intervene,” Drs. Dalton and DeZern concluded. “We cannot improve outcomes for patients through diagnostics alone; we require active, nontoxic interventions to alter the natural history of their MDS – from higher to lower risk disease.”
Reference
DeZern AE and Dalton WB. How low risk are low risk myelodysplastic syndromes? Expert Rev Hematol. 2022;15(1):15-24.




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.