Take-aways:
- Patients with TP53-mutated disease, in general, have poor outcomes, with a two-year overall survival rate of 12.8%.
- TP53-mutated AML and MDS-EB do not differ with respect to their clinical and molecular characteristics or survival outcomes.
- Bi-allelic mutant TP53 status was observed in 174 patients (76%), and multiple TP53 mutations were detected in 49 patients (21%).
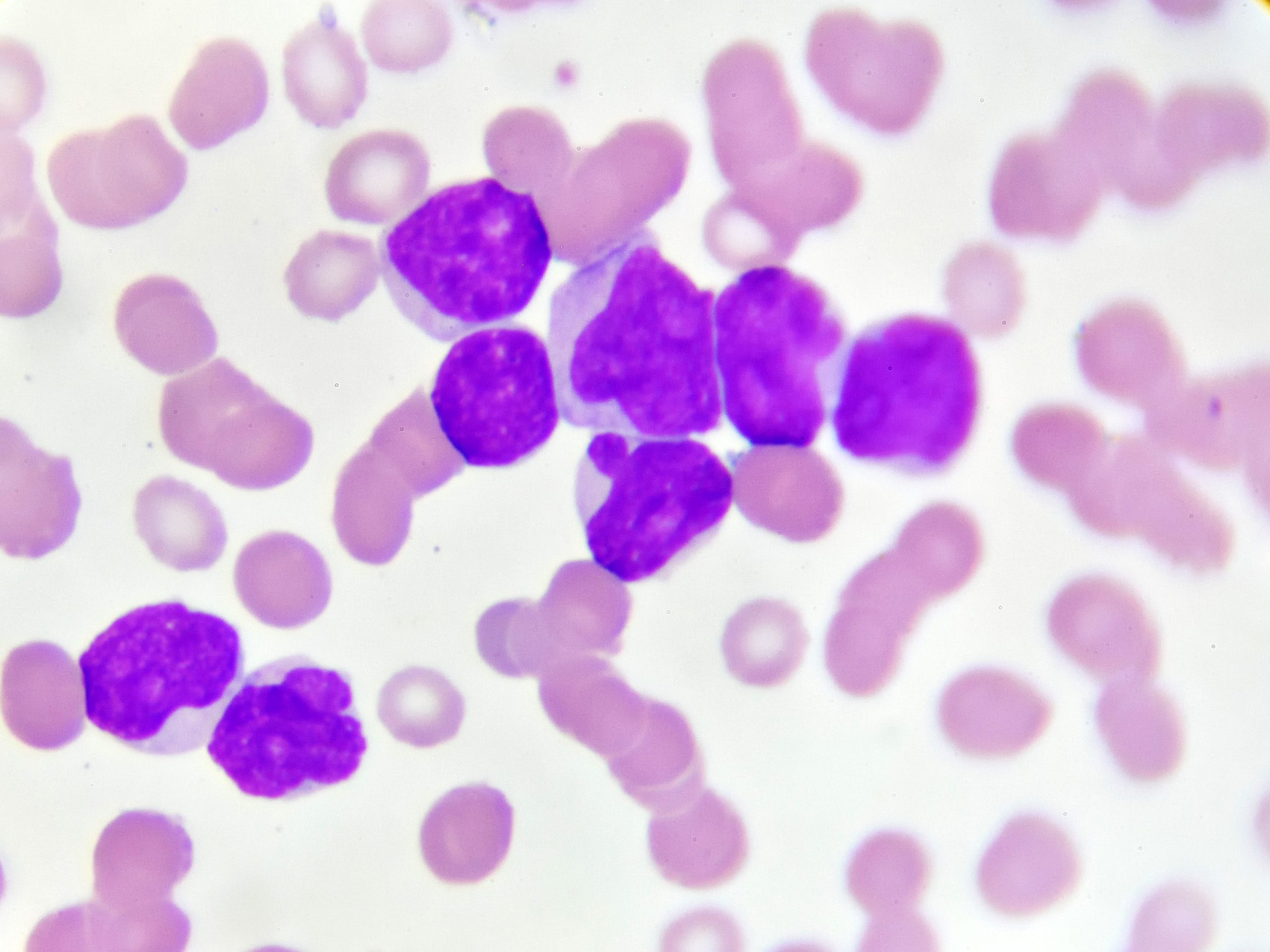
TP53-mutated acute myeloid leukemia (AML) and myelodysplastic syndromes with excess of blast (MDS-EB) do not differ with respect to their molecular characteristics and patient survival outcomes, according to a study published in Blood.
The study, led by Tim Grob, MD, of the Erasmus Medical Center Cancer Institute at the University Medical Center Rotterdam in the Netherlands, suggests that TP53-mutated AML/MDS-EB should be considered a single molecular disease entity rather than treated separately.
“Mutant TP53 AML/MDS-EB represents a molecular homogeneous group with distinct clinicopathologic characteristics and outcomes,” Dr. Grob and colleagues wrote. “Therefore, we propose that mutant TP53 MDS-EB and AML should be considered a single entity, regardless of the requisite blast percentage at diagnosis.”
It was previously unknown whether TP53-mutated AML and MDS-EB differ in their molecular makeup and response to treatment.
Study Cohort
Researchers assessed data from 2,200 patients diagnosed with AML or MDS-EB (defined as International Prognostic Scoring System [IPSS] ≥1.5 or revised IPSS >4.5) undergoing standard induction chemotherapy in the HOVON-SAKK (Haemato-Oncology Foundation for Adults in the Netherlands and Swiss Group for Clinical Cancer Research) clinical trials between 2001 and 2017.
Researchers used next-generation sequencing (NGS) on AML and MDS-EB specimens to identify the molecular characteristics of each in detail and determine their impact on survival.
A total of 283 TP53 mutations were detected in 230 patients (10.5%); 44 patients (19%) were diagnosed with MDS-EB.
The median variant allele frequency was 47%. Bi-allelic mutant TP53 status was observed in 174 patients (76%), and multiple TP53 mutations were detected in 49 patients (21%). Concurrent mutations were detected in 113 patients (49%), with the most frequently concurrent mutations being DNMT3A, TET2, ASXL1, RUNX1, and SRSF2.
TP53-Mutated AML, MDS-EB Indistinguishable
In terms of clinical characteristics, the researchers found that TP53-mutated AML and MDS-EB were indistinguishable with respect to patient age, sex, white blood cell count, remission rate, cytogenetics, and outcomes.
The study found no difference between AML and MDS-EB in terms of overall survival (OS). Patients with TP53-mutated disease, in general, have poor outcomes, with a two-year OS rate of 12.8%.
In terms of molecular characteristics, the researchers found that TP53-mutated AML and MDS-EB were indistinguishable with respect to TP53 mutant allelic status, number of TP53 mutations, mutant TP53 clone size, and concurrent mutations. Furthermore, none of these molecular characteristics were significantly associated with survival in TP53-mutated AML or MDS-EB.
Another important prognostic marker in AML is the detection of TP53-mutated molecular minimal residual disease (MRD). The authors analyzed complete morphological remission bone marrow samples with deep targeted sequencing on 62 patient samples with TP53-mutated AML. In total, 45 bone marrow samples had detectable TP53 mutations in complete remission, which was determined to not be associated with OS (P=.653).
“It is conceivable that all patients with mutant TP53 AML/MDS-EB achieving [complete remission] have MRD, sometimes at levels undetectable with current NGS approaches,” the authors wrote.
Complex Karyotypes
The new study contradicts earlier studies that found significant associations of TP53 mutant allelic status and mutant TP53 clone size with a more favorable outcome for patients with MDS and AML due to the interactions between these molecular characteristics and complex karyotypes (CKs), which are associated with reduced OS in myeloid malignancies.
The authors speculated that the reason they found no such associations was that their analysis did not include patients with low-risk MDS who often associate with non-CK.
In the current study, 84% of patients with TP53-mutated AML/MDS-EB were found to have CK, and numerous associations between CK and the different molecular characteristics were observed.
Looking Ahead
In addition to treating TP53-mutated AML/MDS-EB as a single entity, Dr. Grob and colleagues suggested that further investigation into molecular MRD detection in patients with TP53-mutated AML/MDS-EB would be beneficial.
“Although the applicability of molecular MRD detection in patients with mutant TP53 AML/MDS-EB in our study is limited, future clinical trials with new drugs and other quantified MRD endpoints may benefit from molecular MRD detection based on mutant TP53,” the authors wrote of a limitation of the study.
Accompanying Commentary
In an accompanying commentary by John S. Welch, MD, PhD, of the Washington University School of Medicine in St. Louis, Missouri, published in the same issue of Blood, Dr. Welch describes AML and MDS as “star-crossed lovers” whose diagnostic separation has been the subject of changing guidelines. According to Dr. Welch, clinicians tend to be either “splitters,” who seek to diagnose increasingly narrow groups of patients, or “lumpers” who seek broad, overarching patterns that unite diagnostic classifications. Dr. Welch characterized the paper by Dr. Grob and colleagues as falling under the latter category.
Dr. Welch added that lumping the two diagnoses together may yield diagnostic benefits: “Bringing these diseases t���q�SMB@����������������k~#�����K�����
�<+V������������������1��������������Se����������������������������istent enrollment onto TP53-mutant–focused clinical trials.”
References
Grob T, Al Hinai ASA, Sanders MA, et al. Molecular characterization of mutant TP53 acute myeloid leukemia and high-risk myelodysplastic syndrome. Blood. 2022;139(15):2347-2354.
Welch JS. TP53 and the star-crossed lovers MDS and AML. Blood. 2022;139(15):2265-2266.




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.