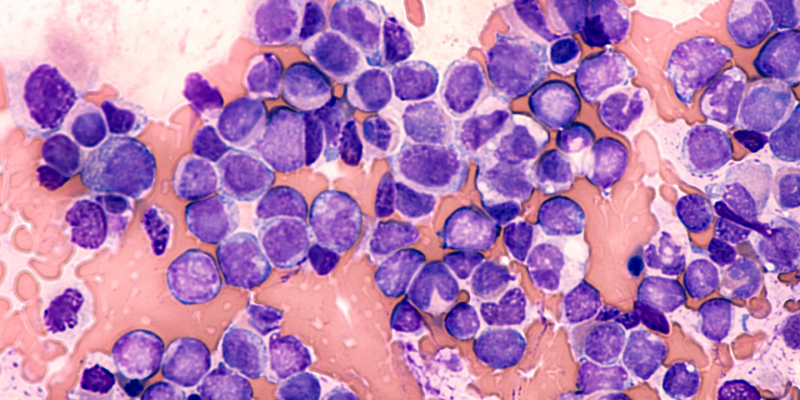
The combination of intravenous ivosidenib and azacitidine produced deep and durable remissions associated with clearance of IDH1-mutated newly diagnosed acute myeloid leukemia (AML), according to results of the AGILE study presented at the 2022 American Society of Hematology Annual Meeting.
Ivosidenib is a potent oral targeted IDH1 mutation inhibitor that is approved by the U.S. Food and Drug Administration (FDA) as a monotherapy for treatment of relapsed/refractory AML and newly diagnosed AML in adults aged older than 75 years or those with comorbidities that preclude intensive chemotherapy. The FDA also recently approved the combination of ivosidenib and azacitidine in older or unfit patients with IDH1-mutated AML.
In the most recent data presented, researchers sought to characterize clonal evolution and relapse in newly diagnosed patients with IDH1-mutated AML treated with this combination.
Researchers used next-generation sequencing to assess 72 patients, 46 of whom had both baseline and longitudinal mutational data available.
The median follow-up was 366 days (range, 16-1,210 days), and the median number of baseline mutations was three (range, 1-10 mutations). Presence of baseline DNMT3A, TET2, and ASXL1 (DTA) mutations were not assessed for clearance due to potential clonal hematopoiesis, the authors noted.
Nearly two-thirds of patients (61%; n=28/46) had suppression of all baseline non-DTA mutations to below the limit of detection, including 65% of patients (n=22/34) who achieved a complete remission (CR) or CR with partial hematologic recovery (CRh). Among patients who did not achieve CR/CRh, the baseline mutation clearance rate was 60% (n=3/5), and among non-responders, the clearance rate was 50% (n=3/6).
To identify potential mechanisms of acquired resistance, on-treatment samples were analyzed for the emergence of mutations not detected at baseline. Emerging mutations were identified in nearly half of patients (48%; n=22/46), with a median of two emerging mutations per patient (range, 1-6 mutations). Two patients (4%) had emerging mutations in IDH2 and discontinued treatment due to adverse events and stable disease, respectively. No second-site IDH1 mutations occurred.
Among the 10 patients who discontinued treatment following an objective response due to relapse, longitudinal samples were available for eight of those patients. Emerging mutations were detected in six of these patients (75%). Genes with emerging mutations recurrently associated with relapse included ASXL1, FLT3, RUNX1, and TET2 (occurring in two patients each). IDH1 mutation was not detected at relapse in six patients (75%). Among the two relapses that occurred in the absence of emerging mutations, one was associated with expansion of a baseline FLT3-ITD subclone, and the other was not associated with any new emerging or expanding mutations.
“To date, no second-site IDH1 mutations have been observed, but mutations in other genes, including IDH2, can emerge and may provide an opportunity for relapse,” the researchers concluded. “Further study is needed to better characterize mechanisms of relapse to ivosidenib plus azacitidine.”
Reference
Döhner H, Marchione DM, Choe S, et al. Molecular characterization of clinical response and relapse in patients with IDH1m ND-AML treated with ivo+AZA in the AGILE study. Abstract #223. Presented at the 64th ASH Annual Meeting and Exposition; December 10-13, 2022; New Orleans, Louisiana.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.