ASH 2024: MDS
Nicole Grieselhuber, MD, PhD on results of SEA-CD70 treatment in patients with high-risk MDS.
An expert panel delves into new data regarding the long-term efficacy of luspatercept in MDS.
An expert MDS panel discusses patient reported outcomes, transfusion dependence, and time toxicity.
Advertisement
The COMMANDS trial evaluated frontline luspatercept in transfusion-dependent patients with lower-risk MDS and anemia.
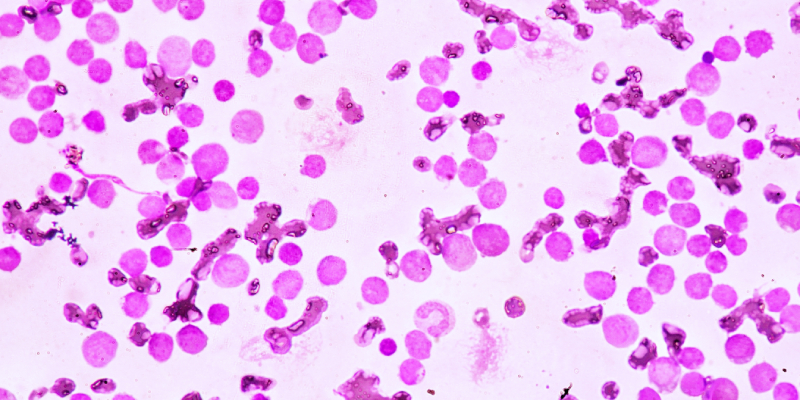
HMAs, either as monotherapy or in combination with venetoclax, represent the standard of care for higher-risk MDS or AML.
According to a study, patients with MDS and CMML have dismal clinical outcomes after failure of HMA therapy.
Advertisement
Investigational combinations for MDS appeared to be well tolerated while triplets results in high-grade toxicity.
An expert speaks on site at ASH 2024 about the health-related quality of life data from the phase 3 COMMANDS trial.
Moving forward, prospective studies must validate these findings and refine risk stratification tools like the IPSS-R in MDS.
Some patients with ZRSR2-mutated CCUS had concurrent blood cancers or disorders, and others had protective co-mutation.
A discussion on the post hoc analysis on quality of life from the COMMANDS trial.
Discussing the COMMANDS trial and sequencing luspatercept in patients with myelodysplastic syndromes.
How to address ESA failure or ineligibility in patients with MDS...
Results from a real-world analysis of post-ESA treatment outcomes in patients with lower-risk myelodysplastic syndrome.
Early signs of clinical activity have been shown in a phase I/II study of tagraxofusp/decitabine in MDS and CMML.
Mature data of three immunotherapy-based hypomethylating agent combinations were presented at ASH.
Interim results suggest acceptable safety and high efficacy of CPX-351 plus ivosidenib.
High complete response rates and low early mortality rates facilitate the majority of patients to allogeneic SCT.
An ongoing phase 1 study is evaluating the safety and efficacy of danvatirsen through two substudies.
HMA plus venetoclax may achieve higher response rates and improve event-free survival in high-risk MDS.







 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.