Survival in patients with NPM1-mutated myeloid neoplasms (MNs) is improved by management approaches used for acute myeloid leukemia (AML). This is according to retrospective study findings presented at the Society of Hematologic Oncology 2024 Annual Meeting in Houston, Texas.
“Our data add to the supporting evidence that NPM1-mutated MNs, even with low marrow blasts, are consistent with AML and benefit from an AML treatment approach,” wrote lead author Brandon Kale, MD, of the Morsani College of Medicine at the University of South Florida in Tampa, Florida.
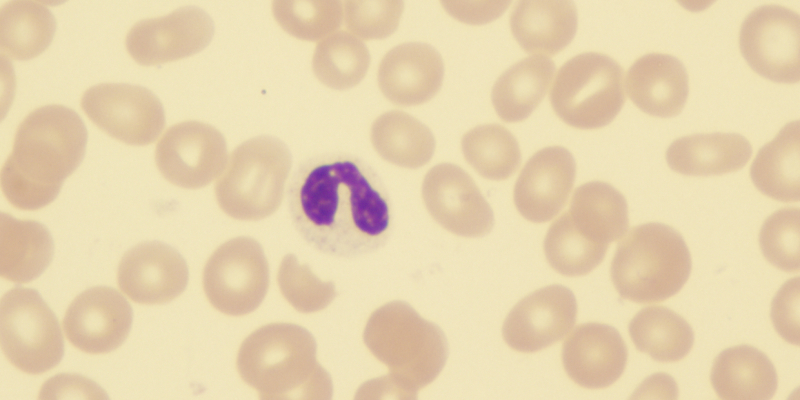
The study evaluated 40 patients at a single center; 30 had NPM1-mutated myelodysplastic syndrome and 10 had chronic myelomonocytic leukemia. Of the total cohort, 55% of patients at diagnosis had bone marrow blasts of less than 10% and 45% had blasts of 10% or more. In addition, 47.5% of patients had high-risk or very high-risk disease as defined by the revised International Prognostic Scoring System. Disease had transformed into AML in 85% of the patients. There were co-mutations of DNMT3A in 35% of patients, TET2 in 25%, IDH1/2 in 20%, FLT3-ITD/TKD in 17.5%, and PTPN11 in 12.5%.
Regarding frontline therapies received by the patients, the study classified cytarabine-based regimens as “intensive” and hypomethylating agent (HMA)-based regimens as “non-intensive,” and the researchers categorized patients accordingly. No patients were under an HMA plus venetoclax regimen. Of the total cohort, 42.5% had received intensive therapy, and the median age for either treatment group was comparable at 68 years (P=0.472). In addition, 40% of the total cohort had undergone allogeneic hematopoietic stem cell transplant (HSCT).
The median overall survival (mOS) calculated for the intensive therapy group was 63 months, compared with 35.2 months in the non-intensive therapy group (P=0.0295). Among patients who had less than 10% marrow blasts, those with intensive therapy did not reach mOS, whereas those with non-intensive therapy had an mOS of 31.2 months (P=0.020). Among patients who had marrow blasts of 10% or more, those with intensive therapy did not reach mOS, whereas those with non-intensive therapy had an mOS of 14.1 months (P=0.030). Patients who had received HSCT had an mOS of 70.8 months compared with 31.1 months in those who had not (P=0.001).
Additional multivariate regression confirmed the effect on patient survival from intensive treatment (hazard ratio [HR] = 0.25; P=0.003) and HSCT (HR = 0.30; P=0.006).
“Evaluation of larger data sets that confirm these observations may help guide future treatment recommendations for these patients,” Dr. Kale observed.
Reference
Kale B, Sallman D, Al Ali N, et al. NPM1-mutated myeloid neoplasms irrespective of blast count are associated with better outcomes with acute myeloid leukemia treatment approach. Abstract #MDS-570. Presented at the Society of Hematologic Oncology 2024 Annual Meeting; September 4-7, 2024; Houston, Texas.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.