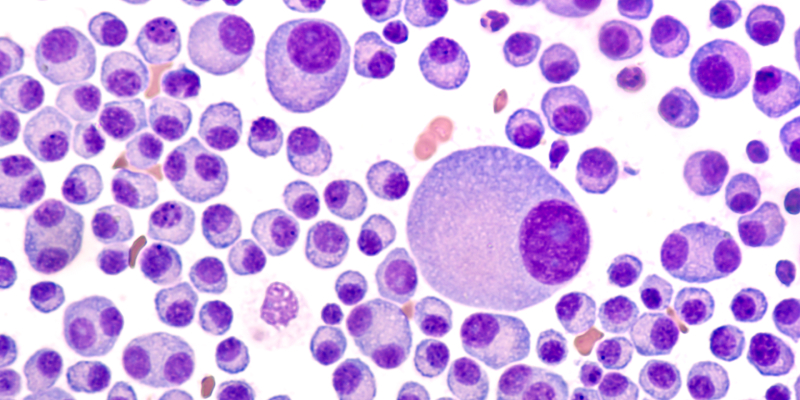
A new study suggests a “significant proportion of interventional phase III clinical trials” that enrolled patients with multiple myeloma (MM) “didn’t clearly define high-risk MM.”
Faris Jamal Abu Za’nouneh, MD, of the Jordan University of Science and Technology, and colleagues conducted the study because of the “concern that a homogenous definition of high-risk MM is not unified in clinical trials.” They presented the study’s results at the 2022 American Society of Hematology Annual Meeting.
It was important to conduct the research because “despite the significant improvement in outcomes for patients with MM, a proportion of patients with high-risk disease features continue to have relatively poor outcomes,” the study’s investigators wrote.
They outlined the International Myeloma Working Group’s definition of high-risk cytogenetic abnormalities, which is “the presence of t(4;14), t(14;16), t(14;20), del(17/17p), or gain(1q) in fluorescence in situ hybridization, nonhyperdiploid karyotype, karyotype del(13) or high-risk signature in gene expression profiling.”
The study’s investigators performed a cross-sectional analysis of all phase III interventional MM clinical trials that were registered at clinicaltrials.gov and found 327 trials, 275 of which were included in the analysis. The median start date for the clinical trials included was 2011 (range, 1998-2021), while the median publication date was 2017 (range, 2006-2022).
The researchers were able to directly extract the definition of high-risk MM from the full publication in 88% of the studies. They obtained the definition of high risk in the remaining 12% from the protocol or data available at clinicaltrials.gov.
“Studies that reported a definition of high-risk were those with higher number of enrolled patients, and those with a full publication,” the authors wrote. “Location of study (US vs others) and funding ([pharmaceutical industry] vs others) were not associated with higher percentage of high-risk definition.”
Of the 275 studies, 99 (36%) “reported the use of at least one definition of high-risk MM,” according to the researchers.
“Few studies used laboratory markers solely in high-risk definitions,” the researchers wrote, noting that beta-2-microglobulin was only used in four studies, while lactate dehydrogenase was only used in one.
Within these 99 studies, 94% defined high-risk MM by cytogenetics, as determined by fluorescence in situ hybridization, or karyotype, while four studies included definitions of International Staging System scores stage II or III as high-risk. Another four studies used gene expression profiling in the definition of high-risk MM. The International Myeloma Working Group’s definition of high-risk MM was followed in 10% of the studies. Of the 99 studies, 10% used more than one criterion in the high-risk MM definition.
“Our analysis indicated that a significant proportion of interventional phase III clinical trials in MM didn’t clearly define high-risk MM and when defined, the definition used was heterogenous and largely not based on certain thresholds of cytogenetic abnormalities,” the researchers concluded. “A unified definition that includes all proven clinical and/or disease high-risk features is needed for future clinical trials.”
Reference
Abu Za’nouneh F, Ababneh O, Schinke C, et al. Variability of definition of high-risk multiple myeloma in phase III clinical trials. Abstract #4545. Presented at the 64th ASH Annual Meeting and Exposition; December 10-13, 2022; New Orleans, Louisiana.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.