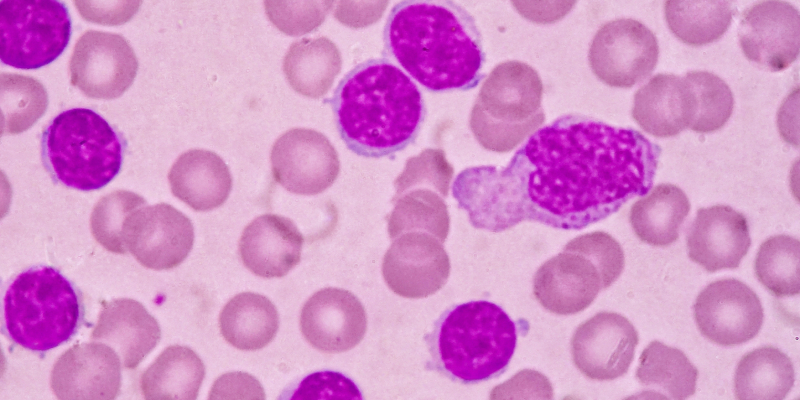
Chronic lymphocytic leukemia (CLL) constitutively overexpresses the B-cell lymphoma 2 (BCL2) protein and related family proteins, resulting in dysregulation of normal intrinsic apoptosis and ultimately in inhibition of cell death. Therapeutic use of BCL2 inhibitors (eg, venetoclax) in CLL, as both continuous monotherapy or in a fixed-duration combination, has resulted in clinical benefit with significant rates of complete responses (CRs), including those without detectable minimal residual disease (MRD).
This review seeks to describe both the disease factors that influence primary venetoclax sensitivity and resistance and those resistance mechanisms that may be acquired secondary to BCL2 inhibitor therapy in CLL and proposes future applications of BCL2 inhibitor therapy in CLL and potential means by which BCL2 inhibitor-resistance may be abrogated.
Therapeutic BCL2 Inhibition
BCL2 is now an established therapeutic target in the treatment of CLL. The selective BCL2 inhibitor venetoclax demonstrated considerable overall response rates (ORRs) and CR rates in early-phase monotherapy clinical trials treating lymphoid malignancies, including CLL, and importantly including a small number of MRD-negative remissions. When venetoclax is administered in combination with anti-CD20 monoclonal antibodies or a Bruton’s tyrosine kinase (BTK) inhibitor, the rates of undetectable MRD CRs observed in CLL appear to be augmented. Fixed-duration venetoclax combination therapy is now an emerging standard of care in the treatment of both frontline and relapsed/refractory CLL.
However, differential baseline sensitivity to venetoclax therapy between lymphoid neoplasms and among CLL patients has been repeatedly observed. In addition, most patients who are continuously exposed to venetoclax following an initial response will eventually develop secondary resistance.
The balance and interactions between BCL2 family member proteins determine whether apoptosis may occur. Intrinsic cellular apoptosis may be induced in normal circumstances by the antagonistic binding of BH3-only proteins to anti-apoptotic BCL2 at the BH3-binding groove, which releases the restraints on BAX/BAK. When BCL2 is overexpressed in CLL, the consequent sequestration of pro-apoptotic proteins tips the balance of BCL2 family proteins toward cell survival.
Intrinsic Sensitivity/Resistance to Venetoclax
Baseline venetoclax sensitivity or resistance is influenced by the expression of BCL2 relative to other BCL2 family member proteins, microenvironmental factors such as nodal T-cell stimulation, and tumoral heterogeneity.
Perhaps the most fundamental factor conferring tumoral sensitivity to BCL2 inhibition is the degree of constitutional BCL2 expression and dependence upon the protein for survival. In general, malignancies of mature B lymphocytes exhibit upregulated BCL2 and also dependence upon the protein. However, upregulation of BCL2 alone does not universally correlate with marked sensitivity to BCL inhibitor therapy. There are likely other mechanisms at play, including dysregulation of other BCL2 family proteins such as BCL-W.
Stimulation by microenvironmental agonists, including those via T-cell stimulation, likely contribute to upregulated nuclear factor kappa B (NF-kB) signaling with secondary baseline increase in antiapoptotic BCL2 family proteins such as BCL-XL and MCL1. Those cells with higher baseline levels of BCL-XL cells due to CD40 signaling are less sensitive to venetoclax, even when combined with anti-CD20. The observation that those patients with higher volumes of residual nodal disease post-venetoclax therapy appear to have shorter progression-free survival (PFS) may attest to the importance of the microenvironment in determining venetoclax resistance.
Secondary Resistance: CLL-Type Progression
With selection pressure applied by continuous venetoclax exposure, secondary resistance mechanisms develop in oligoclonal fashion. Those mechanisms include acquisition of BCL2 variants, dynamic aberrations of alternative BCL2 family proteins, and mutations affecting both BAX and other BH3 proteins.
The discovery of mutations within BCL2 is considered to be a major advance in understanding the mechanisms of secondary venetoclax resistance. The first-in-human venetoclax-induced BCL2 variant discovered was Gly101Val. The discovery followed targeted amplicon next-generation sequencing of the entire BCL2 gene from paired pre- and post-venetoclax patients’ samples from early-phase venetoclax clinical trials.
The survival of CLL cells appears to correlate with upregulation of BCL2 family proteins, particularly MCL1 and BCL-XL. Baseline differential dependence upon particular BCL2 family proteins has been well described between lymphoid malignancies. The balance and interactions among BCL2 family proteins is additionally affected by continuous venetoclax exposure and underpins an important feature of drug resistance.
BCL-XL is likely more heavily implicated in venetoclax resistance than MCL1. Direct co-inhibition of BCL-XL and BCL2 by combination BH-3 mimetics in venetoclax-resistant CLL cell lines is seen to abrogate venetoclax resistance more effectively than co-inhibition of BCL2 and MCL1. In addition, in the presence of BCL2 inhibition, BCL-XL appears to bind BIM preferentially to MCL1. These findings are collectively suggestive of a functional hierarchy among BCL2 family proteins under venetoclax therapeutic pressure.
Future Therapeutic Strategies to Optimize BCL2 Inhibition
It is probable that the duration of venetoclax selection pressure to a heterogeneous CLL tumor environment is an important determinant of emergence of BCL2 resistance mutations. In contrast to continuous venetoclax therapy, combinations with anti-CD20 monoclonal antibodies have not been seen to select for BCL2 resistance mutations.
Mechanistically, the venetoclax-killing effect may be enhanced in combination with a second agent and may allow for fixed-duration venetoclax exposure. Patients with detectable MRD at the end of fixed-duration therapy appear to have shorter PFS, independent of other response observed. Combination therapies appear to augment rates of CR and, importantly, rates of undetectable MRD over those seen with continuous venetoclax monotherapy in early clinical trials.
There is a strong theoretical rationale for therapeutic combinations in the setting of oligoclonal resistance mechanisms. BTK inhibitor therapy and anti-CD20 monoclonal antibodies demonstrate synergism with venetoclax due to a posited increase in CLL cellular BCL2 dependence and downregulation of microenvironmental signaling. However, many questions remain regarding the optimal combinations and sequencing of targeted therapies in CLL.
A less understood area of growing interest is the potential utility of targeting the mechanisms of venetoclax resistance and even the microenvironment in which venetoclax-resistant clones may be selected for. Due to their roles in resistance previously described, potential targets under evaluation include MCL1, BCL-XL, and epigenetic modifiers, along with manipulation of NF-kB and PI3K/AKT/mTOR pathways.
In addition to these approaches seeking to abrogate resistance at treatment outset, a second yet untested approach could add an appropriate second agent as dominant resistant clones emerge under serial molecular evaluation.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.