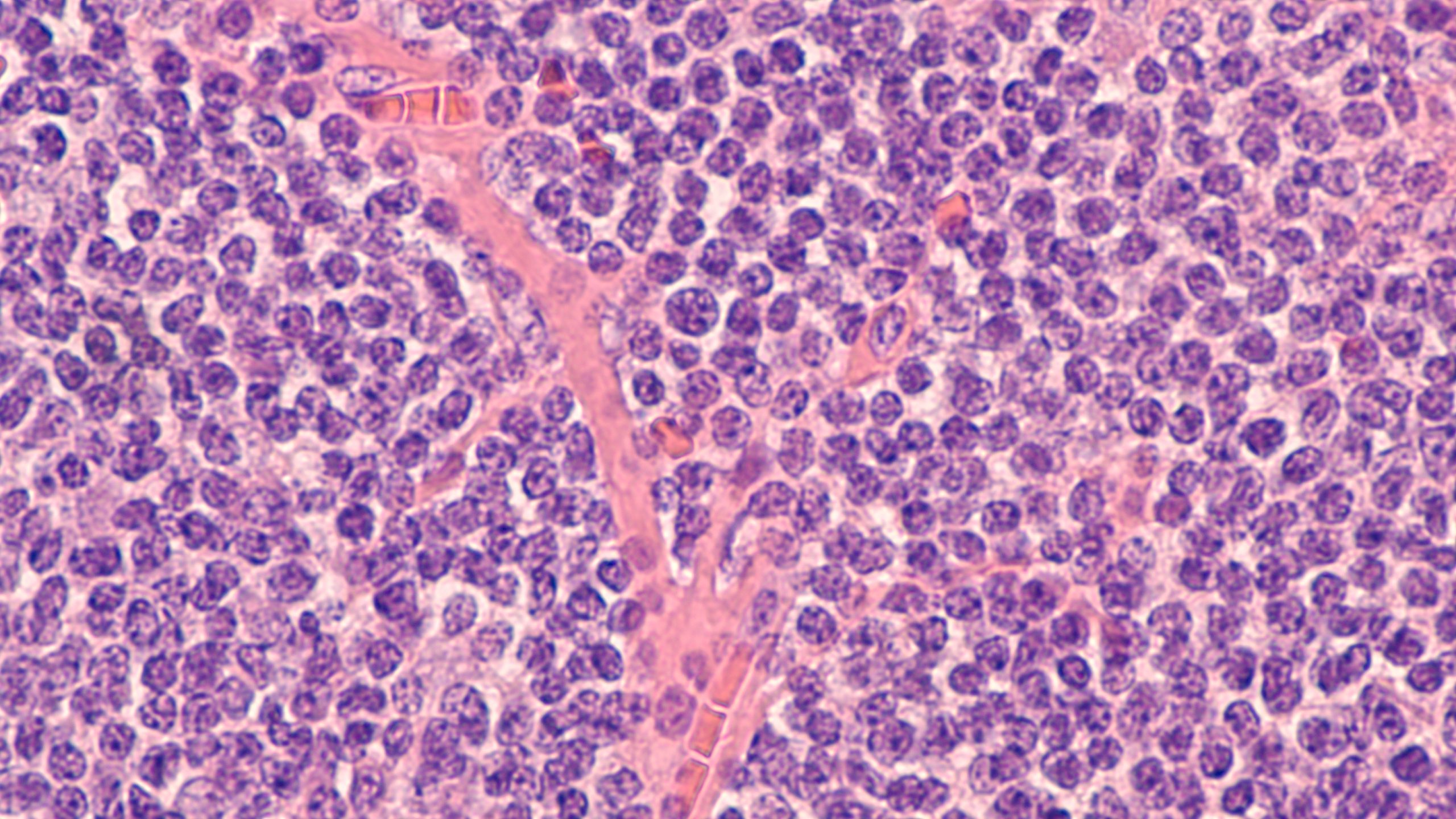
Mantle cell lymphoma (MCL) is associated with a poor prognosis and is rarely curable with currently available standard treatment. Regardless of the initial therapy received, most patients will eventually relapse and go on to receive multiple lines of subsequent therapies.
This article discusses current strategies for managing relapsed MCL. Topics include the use of targeted therapies such as Bruton’s tyrosine kinase (BTK) inhibitors, lenalidomide, bortezomib, and venetoclax; the role of hematopoietic stem cell transplantation (HSCT) and chimeric antigen receptor (CAR) T-cell therapy; and the development of emerging therapies such as bispecific T-cell engagers (BiTEs) and antibody-drug conjugates (ADCs).
Retreatment with Chemotherapy
Patients who have an extended duration of response to first-line chemoimmunotherapy—particularly those who exceed the expected median progression-free survival with first-line therapy—can be effectively treated with an alternative chemotherapy regimen at first relapse.
The authors currently consider a regimen of bendamustine plus rituximab in patients who have a prolonged first remission and no prior bendamustine exposure, especially patients who are ineligible for oral agents. However, patients who relapse within two years of first-line chemoimmunotherapy and those with other high-risk disease characteristics such as TP53 aberrations are best managed using alternative treatment approaches.
BTK Inhibitors
The pharmacologic inhibition of BTK results in anti-tumor activity in several B-cell malignancies, including MCL. At present, three irreversible BTK inhibitors—ibrutinib, acalabrutinib, and zanubrutinib—are approved by the U.S. Food and Drug Administration (FDA) for the treatment of relapsed/refractory MCL.
Unless a patient is eligible for a clinical trial, the authors’ current approach is to treat with a BTK inhibitor at the time of first relapse. There are currently no prospective, head-to-head comparisons of the BTK inhibitors in MCL, so the choice of medication is generally based on consideration of the side effect profile and patient factors. However, emerging data from prospective trials of BTK inhibitors in other B-cell malignancies suggest that the second-generation BTK inhibitors are better tolerated than ibrutinib.
Lenalidomide
Lenalidomide is an oral immunomodulatory agent that is thought to stimulate T-cell and natural killer cell anti-tumor activity while also inhibiting oncogenic processes in the tumor microenvironment such as tumor-associated angiogenesis. It is currently FDA-approved for the treatment of relapsed/refractory MCL based on the results of multiple clinical trials that reported modest single-agent activity.
For patients with relapsed/refractory MCL who did not receive lenalidomide in the first-line setting, the authors consider using a combination of lenalidomide and rituximab for patients who experience progression on a BTK inhibitor. They also use this regimen in patients who are ineligible for CAR-T therapy or clinical trials, although responses in this setting are often short lived. They do not routinely use lenalidomide as a single agent or in other combination regimens outside of a clinical trial.
Bortezomib and Other Proteasome Inhibitors
Bortezomib is currently FDA-approved for relapsed/refractory MCL. While bortezomib continues to have a role in the first-line treatment of MCL as part of the bortezomib plus rituximab, cyclophosphamide, doxorubicin, and prednisone regimen, the modest single-agent response rates and increased toxicity seen with combination regimens limit its use in the relapsed/refractory setting, especially with the availability of more active agents like BTK inhibitors and CAR-T.
Ixazomib, another proteasome inhibitor, is available in an oral formulation and is associated with lower rates of peripheral neuropathy compared with bortezomib. While ixazomib is not currently indicated for use in MCL, combination regimens such as ixazomib plus ibrutinib and ixazomib plus rituximab are currently under investigation for patients with relapsed disease.
Venetoclax
Venetoclax is an oral B-cell lymphoma 2 inhibitor that is currently FDA-approved for the treatment of chronic lymphocytic leukemia and acute myeloid leukemia. Due to the relatively low response rates and poor overall survival associated with venetoclax in relapsed/refractory MCL, this agent is currently best used as a bridge to more definitive therapy rather than a long-term treatment approach. The authors consider the use of venetoclax in select patients who progress after treatment with a BTK inhibitor to achieve disease control prior to CAR-T.
CAR T Cells
Brexucabtagene autoleucel is an anti-CD19 autologous CAR-T product with a CD28 costimulatory domain that is now FDA-approved for the treatment of relapsed/refractory MCL. Another autologous anti-CD19 CAR-T product, lisocabtagene maraleucel, is currently FDA-approved for the treatment of relapsed/refractory large B-cell lymphomas but is not yet approved for patients with MCL.
The authors currently use CAR-T in patients after progression on a BTK inhibitor. Not all patients will be eligible for CAR-T due to toxicity, but studies of patients with other B-cell non-Hodgkin lymphomas (NHLs) treated with CAR-T suggest that this therapy is well tolerated even in older adults. Bridging therapy is often required while waiting the two to three weeks for product manufacturing. The authors typically use corticosteroids, BTK inhibitors, venetoclax, or lenalidomide and rituximab depending on prior therapies a patient has received and how aggressive the disease is at time of progression. Patients with rapidly progressive disease may require combination chemotherapy for bridging.
Allogeneic HSCT
Allogeneic HSCT is a potentially curative treatment option for patients with multiply relapsed MCL, although high rates of serious adverse events and treatment-related mortality limit the use of this approach. Patients who remain medically fit after receiving multiple lines of therapy can be considered for allogeneic HSCT, and this approach can lead to long-term remissions in up to 30% of patients.
There is a lack of data for patients with MCL who proceed to allogeneic HSCT once they have had progressive disease after CAR-T. However, a small number of patients with other subtypes of B-cell NHL proceeded to allogeneic HSCT after failing CAR-T therapy on the ZUMA-1 and JULIET trials, and this approach is currently supported by expert opinion. Based on this information, the authors’ current practice is to consider allogeneic HSCT in fit, motivated patients with MCL who relapse after receiving CAR-T.
Emerging Therapies
BiTE antibodies simultaneously target antigens on malignant cells and T cells, which brings host immune effector cells near tumor cells and triggers cell-mediated cytotoxicity. These agents have the advantage of being off-the-shelf products and are thus more readily available, whereas CAR T cells can take weeks to manufacture, which may limit their use in patients with rapidly progressive disease.
ADCs have also emerged as a promising class of agents for the treatment of MCL and other lymphomas. Polatuzumab vedotin is an ADC-targeting CD79b currently FDA-approved for the treatment of relapsed/refractory diffuse large B-cell lymphoma.
Conclusions and Recommended Treatment Approach
Clinical trial enrollment should be considered at any point when managing patients with relapsed/refractory MCL. If a suitable trial is not available, BTK inhibitors are the preferred class of agent to use at the time of first relapse, especially in patients who have a short duration of response (less than 24 months) to first-line chemoimmunotherapy or those with high-risk disease characteristics like TP53 aberrations. The choice of BTK inhibitor is generally based on consideration of patient comorbidities and the side effect profile of each available agent, and patients who are intolerant to one BTK inhibitor can potentially trial an alternative agent.
The authors occasionally consider retreatment with chemotherapy, often with the bendamustine and rituximab regimen, in patients who achieved prolonged remission with first-line chemotherapy, have no prior bendamustine exposure, and are interested in receiving time-limited therapy as opposed to indefinite treatment with an oral agent. They then consider CAR-T in eligible patients who experience disease progression while on treatment with a BTK inhibitor, as this treatment is associated with high response rates even among patients with high-risk disease.
The prognosis remains poor for patients who are ineligible for CAR-T, as other standard-of-care options in this setting are often unable to produce long-term remissions. If no suitable clinical trial options are available, the authors consider use of the lenalidomide and rituximab regimen and venetoclax for these patients. Lastly, they consider allogeneic HSCT in fit patients who progress after CAR-T.



 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.