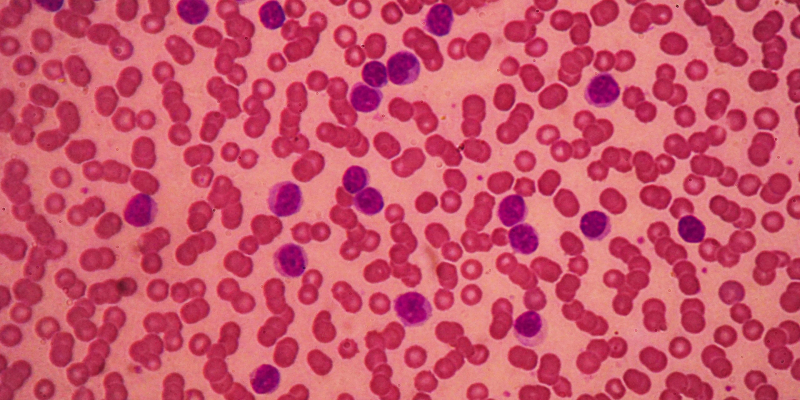
Zanubrutinib continues to outperform ibrutinib in terms of efficacy among patients with relapsed or refractory chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL), and zanubrutinib has an enhanced safety and tolerability profile.1
“The key takeaway is not only is zanubrutinib more effective than ibrutinib in the setting of relapsed CLL, with higher response rates and longer progression-free survival [PFS], but also has significantly less atrial fibrillation, a significant cardiac side effect in patients with CLL,” Susan O’Brien, professor in the Division of Hematology/Oncology, Department of Medicine, UCI Health, told Blood Cancers Today.
The findings come from the phase III ALPINE study (NCT03734016), which revealed the superiority of zanubrutinib over ibrutinib in the primary analysis.1,2 At a median follow-up of 29.6 months, zanubrutinib showed a 32% reduction in the risk of disease progression or death versus ibrutinib (hazard ratio [HR], 0.65; 95% CI, 0.49-0.86; P =.002).2 Extended follow-up was conducted for 652 patients with relapsed or refractory CLL or SLL. Patients were randomized 1:1 to received zanubrutinib, 160 mg twice daily, or ibrutinib, 420 mg once daily, with no possibility of crossover.1
At a median follow-up of 42.5 months, the PFS rate at 36 months was 65.4% with zanubrutinib versus 54.4% with ibrutinib (HR, 0.68; 95% CI, 0.54-0.84). The PFS benefit of zanubrutinib over ibrutinib was maintained across select subgroups including high-risk patients with 17p deletions (del[17p]) or TP53 mutations (HR, 0.79; 95% CI, 0.61-1.02). According to sensitivity analyses, the PFS benefit observed with zanubrutinib in the study may have been associated with antileukemic effect and tolerability.
The overall survival (OS) rates at 36 months were 82.6% in the zanubrutinib arm compared with 79.7% in the ibrutinib arm. The median OS was not reached for either group, but results showed that 21.1% of the zanubrutinib arm had died at the time of data cutoff compared with 25.5% of the ibrutinib arm (HR, 0.77; 95% CI, 0.55-1.06).1
Zanubrutinib also demonstrated a higher objective response rate (ORR) of 85.6% compared with a 75.4% ORR with ibrutinib (response ratio, 1.13; 95% CI, 1.05-1.22). Responses to Bruton tyrosine kinase inhibitor (BTKi) therapy deepened over time in both treatment arms; however, complete responses (CR) and CR with incomplete count recovery were only achieved in patients treated with zanubrutinib.
Observing safety year over year in the ALPINE study, investigators reported that the majority of adverse events were stable. Between the 36- and 48-month time points, the most common adverse events in the zanubrutinib arm versus the ibrutinib arm were infections (49.5% vs 45.1%), hypertension (21.5% vs 20.6%), COVID-19 (22.9% vs 13.7%), and bleeding (19.6% vs 21.7%).
As a result of sustained benefit after 3 years of treatment in the zanubrutinib arm, investigators decided to close the ALPINE study, allowing eligible patients originally assigned to receive ibrutinib to enroll in the LTE1 study (NCT04170283), which investigates zanubrutinib monotherapy in patients with B-cell malignancies.
“The final impact of the ALPINE study is that physicians will be more likely to choose zanubrutinib as their go-to BTKi in CLL,” said O’Brien.
References
- Brown J, Eichhorst B, Lamana N, et al. Sustained benefit of zanubrutinib vs ibrutinib in patients with R/R CLL/SLL: final comparative analysis of ALPINE. Blood. 2024;144(25):2706-2714. doi: 10.1182/blood.2024024667
- Brown J, Eichhorst B, Hillmen P, et al. Zanubrutinib or ibrutinib in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med. 2023;388(4):319-332. doi: 10.1056/NEJMoa2211582





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.